
Subscribe to our
Heart surgery is a complex and critical medical procedure that can save lives, restore health, and improve quality of life. However, not every heart condition requires surgery. Sometimes, lifestyle changes, medications, or less invasive treatments may be enough to manage the condition. Let’s explore when heart surgery is necessary, the different types of heart surgeries, how to prepare for them, and the risks involved.
Book an appointment by Clicking Here with our renowned heart surgeons at Felix Hospital today and take the first step towards a healthier heart!
Heart surgery becomes necessary when less invasive treatments cannot effectively manage a condition that threatens the function of the heart. The decision to undergo surgery depends on several factors, including the severity of the heart condition, the overall health of the patient, and the potential benefits of surgery compared to other treatment options.
1. Coronary Artery Disease (CAD): When the arteries that supply blood to the heart become narrowed or blocked due to the buildup of plaque, it can result in chest pain (angina), heart attacks, and other serious complications. If lifestyle changes, medications, and other interventions like angioplasty don’t resolve the problem, coronary artery bypass graft (CABG) surgery may be required.
2. Heart Valve Disease: Heart valves regulate blood flow within the heart. Surgery may be needed to repair or replace the valve when it becomes damaged or diseased (due to infection, aging, or congenital conditions). Severe valve problems can lead to heart failure if not treated surgically.
3. Aortic Aneurysm: A weakened section of the aorta (the main artery in the body) can lead to an aortic aneurysm, which may rupture if left untreated. Surgery is often required to repair the aneurysm to prevent life-threatening internal bleeding.
4. Arrhythmias (Irregular Heartbeats): Certain arrhythmias, like atrial fibrillation, can often be managed with medications or procedures such as catheter ablation. However, in more severe cases, surgical interventions like the Maze procedure or the installation of a pacemaker may be required.
5. Congenital Heart Defects: Some people are born with structural heart problems that may need correction through surgery. Congenital heart defects like holes in the heart, malformed valves, or abnormal blood vessels can cause serious issues if not treated, sometimes requiring immediate surgery in newborns or infants.
6. Heart Failure: Advanced heart failure may require heart transplantation or surgery to implant a ventricular assist device (VAD) to help the heart pump blood effectively.
Not all heart conditions require surgery. Many heart problems can be managed through:
When surgery is necessary, several types of procedures may be recommended, depending on the specific heart condition:
1. Coronary Artery Bypass Graft (CABG) Surgery:
CABG is the most common type of heart surgery, performed to improve blood flow to the heart muscle. It involves taking a healthy artery or vein from another part of the body and using it to bypass the blocked or narrowed coronary artery.
2. Heart Valve Repair or Replacement:
Surgeons can either repair the damaged valve or replace it with a mechanical or biological valve. Valve repair is generally preferred because it preserves the patient's tissue, but sometimes replacement is necessary if the valve is too damaged.
3. Pacemaker or Implantable Cardioverter Defibrillator (ICD) Placement:
A pacemaker or ICD is implanted to help regulate abnormal heart rhythms. These devices monitor the heart's rhythm and deliver electrical impulses or shocks to maintain a normal rhythm.
4. Aortic Aneurysm Repair:
Surgery to repair an aortic aneurysm typically involves replacing the weakened section of the aorta with a synthetic graft. This prevents the aneurysm from rupturing and causing internal bleeding.
5. Maze Procedure:
The Maze procedure is used to treat atrial fibrillation by creating a pattern of scar tissue on the heart that disrupts the abnormal electrical signals causing the arrhythmia.
6. Heart Transplant:
For patients with end-stage heart failure, a heart transplant may be the only option. In this procedure, the patient’s diseased heart is replaced with a healthy donor heart.
Preparation for heart surgery involves both physical and mental readiness, and understanding the heart surgery cost in Noida is an essential part of planning for the procedure. Below are the key steps that patients should take before undergoing heart surgery:
1. Consultation and Evaluation:
Patients will undergo a thorough evaluation, including blood tests, imaging studies, and heart function tests like echocardiograms or stress tests. These help the surgical team assess the patient's health and create a personalized treatment plan.
2. Discuss Medications:
Inform your doctor of all medications you’re taking, including prescription drugs, over-the-counter medicines, and supplements. Certain medications may need to be stopped or adjusted before surgery to reduce any risks.
3. Lifestyle Adjustments:
Patients are often advised to make lifestyle changes, such as quitting smoking, following a heart-healthy diet, and engaging in regular exercise. These steps can help improve overall health and reduce surgery-related risks.
4. Mental Preparation:
The emotional aspect of surgery is significant. It's important to mentally prepare by discussing concerns with healthcare providers, seeking support from family or support groups, or considering counseling to manage any pre-surgery anxiety.
5. Post-Surgery Support:
Plan for the recovery phase by arranging transportation from the hospital, ensuring that you have someone available to assist at home, and becoming familiar with the expected recovery timeline and care needs.
Like any major surgery, heart surgery comes with risks. Understanding these risks is crucial for informed decision-making. The common risks associated with heart surgery include:
1. Infection: As with any surgery, there is a risk of infection at the incision site or in the heart itself.
2. Bleeding: Bleeding during or after surgery is a potential complication. Sometimes additional surgery may be needed to control the bleeding.
3. Blood Clots: Blood clots can form after surgery, which may lead to a stroke or heart attack if they travel to the brain or heart.
4. Arrhythmias: Abnormal heart rhythms can develop after surgery, requiring medication or further treatment.
5. Lung or Breathing Issues: Some patients may experience difficulty breathing or lung complications after heart surgery, particularly if they have pre-existing lung conditions.
6. Kidney Issues: Heart surgery can sometimes lead to temporary or permanent kidney damage, particularly in patients with pre-existing kidney problems.
7. Stroke: There is a small risk of stroke during or after heart surgery, especially in patients who have other risk factors such as high blood pressure or diabetes.
8. Heart Attack: In rare cases, a heart attack can occur during or after heart surgery due to reduced blood flow to the heart.
9. Death: While advances in surgical techniques have greatly improved the safety of heart surgery, there is still a small risk of death, especially in high-risk patients.
When it comes to heart surgery, the expertise and care of your surgeon are of utmost importance. At Felix Hospital, we are proud to have a team of highly skilled and Best heart surgeons in Noida who are dedicated to providing top-quality cardiac care. Meet our distinguished heart specialists:
Dr. Rahul Arora – Senior Cardiothoracic Surgeon
With years of experience in cardiothoracic surgery, Dr. Rahul Arora is known for his precision and expertise in performing complex heart surgeries, including coronary artery bypass grafting (CABG), valve repairs, and congenital heart defect corrections.
Dr. Siddharth Samrat – Cardiac Surgeon
Dr. Siddharth Samrat brings a wealth of knowledge and expertise in managing a wide range of cardiac conditions, from coronary artery disease to heart failure.
Contact Felix Hospital at +91 9667064100 to learn more about our advanced heart care services and how we can help you or your loved one.
Heart surgery is a life-saving procedure for many patients with serious heart conditions. However, not every heart issue requires surgery, and many can be managed with lifestyle changes, medications, or less invasive treatments. For those who do need surgery, understanding the procedure, how to prepare, and the potential risks is critical to achieving the best outcome.
As the Best heart surgery Hospital in Noida, we specialize in providing comprehensive heart care, from diagnosis to advanced surgical treatments. If you or a loved one is facing heart surgery, our team of experienced cardiologists and surgeons are here to guide you through every step of the process.
1. What are the most common types of heart surgeries?
The most common heart surgeries include coronary artery bypass graft (CABG) surgery, valve repair or replacement, and pacemaker or ICD implantation.
2. Can heart conditions be treated without surgery?
Yes, many heart conditions can be managed with medications, lifestyle changes, and minimally invasive procedures.
3. How long does recovery from heart surgery take?
Recovery times vary depending on the type of surgery, but it generally takes 6 to 12 weeks for most patients to recover.
4. What is the survival rate for heart surgery?
The survival rate depends on the patient’s overall health and the complexity of the surgery, but most heart surgeries have a high success rate.
5. Are there alternatives to open-heart surgery?
Yes, minimally invasive techniques like angioplasty and TAVR are alternatives to open-heart surgery for certain conditions.
6. What are the risks of heart surgery?
Risks include infection, bleeding, blood clots, arrhythmias, and stroke, though these are relatively rare with modern surgical techniques.
7. What lifestyle changes should I make before heart surgery?
Patients are often advised to quit smoking, eat a healthy diet, and exercise regularly before surgery.
8. How do I choose the right heart surgeon?
Choose a surgeon who specializes in the procedure you need, has extensive experience, and is part of a reputable medical facility.

Pacemakers have been an essential tool in cardiology, providing life-saving intervention for individuals with arrhythmias and other heart conditions. Traditionally, pacemakers involve a complex system with leads, a pulse generator, and extensive surgical implantation. However, the advent of wireless pacemakers has revolutionized the field, offering numerous advantages over conventional systems. This article explores why wireless pacemakers are considered a game changer for heart patients.
For those considering this innovative treatment, it's important to consult with the best Pacemaker Surgeon in Noida to ensure the highest level of expertise and care. The right surgeon can make a significant difference in the success of the procedure and the overall outcome for the patient.
Contact Felix Hospital today at 9667064100 for personalized care and cutting-edge solutions.
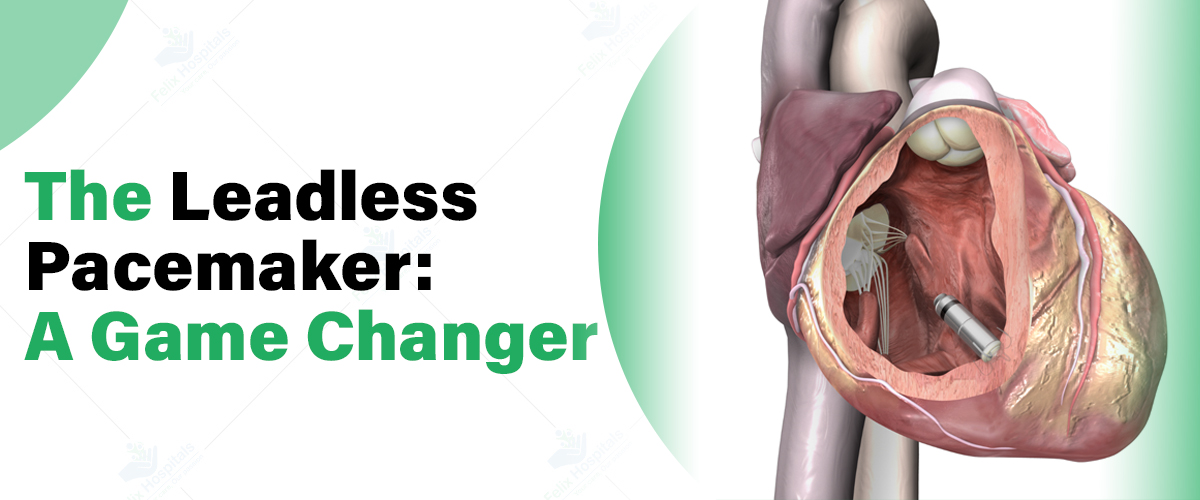
A wireless pacemaker, also known as a leadless pacemaker, is a small, self-contained device implanted directly into the heart via a minimally invasive procedure. Unlike traditional pacemakers, which require leads (wires) to connect the device to the heart, wireless pacemakers are entirely self-contained within the heart chamber. This innovative technology eliminates many of the complications associated with conventional pacemaker systems.
If you're considering Pacemaker Implantation Surgery treatment for heart rhythm disorders, choosing a specialized hospital with expertise in this cutting-edge technology is crucial for optimal outcomes.
1-Decreased chance of complications
Using pacemakers has an additional advantage when it comes to minimizing the risk of complications associated with traditional pacemakers that use leads connected through veins to the heart. These leads are prone to issues like fractures, infections or displacement. Unlike models, modern wireless pacemakers eliminate the need for leads altogether, reducing the likelihood of these complications and ensuring a safer and more efficient treatment for patients by minimizing variations in observation both within and between patients.
2. Minimally Invasive Procedure
Implantation of a pacemaker is considered to be less invasive compared to the traditional wired pacemaker method.The process involves inserting the device through a catheter accessed from the vein directly into the right ventricle of the heart.This approach results in reduced bruising for the patient and typically requires healing time; in some cases it can even be performed as an outpatient procedure.This invasive option is particularly beneficial for patients with underlying health conditions that make them unsuitable, for standard pacemaker surgery.
3. Enhanced Aesthetic and Comfort
The wireless pacemakers are significantly smaller than the ones and can be as small as a large vitamin capsule when it comes to size measurement. One major advantage is that this device is implanted directly onto the heart without requiring a pocket and leads; thus there is no visible swelling under the skin that is often a concern, with most pacemakers. Patients experience comfort as there are no leads or external components that could potentially cause discomfort or irritation.
4. Improved Battery Life
The extended lifespan of the battery in pacemakers is a significant advantage that sets them apart from the traditional ones. These compact devices boast a battery life of 10 to 12 years. Even longer without the need for frequent replacements compared to conventional pacemakers. Moreover the absence of leads allows the battery to consume power leading to a longer lasting battery. This benefit translates into surgical interventions, for patients reducing the chances of complications and easing the overall care burden.
5. Simplified Follow-Up Care
PACEMAKERS play a role in simplifying patient care tasks and are particularly helpful for follow up inquiries with patients. The absence of leads reduces the likelihood of complications that might require monitoring in the future. Moreover; many wireless pacemakers now come with monitoring capabilities that enable doctors to monitor the devices functionality and the patients heart rate without the need for physical check ups. This remote monitoring not only enhances patient comfort but also provides healthcare providers with continuous data to closely monitor and intervene in the patient's condition when necessary.
6. Broader Patient Eligibility
Traditional pacemakers may not work well for every patient those with anatomical issues or increased infection risks. Wireless pacemakers offer an invasive way to implant the device and are beneficial for patients who were unable to get a regular pacemaker due to lead removal concerns. The updated criteria are especially helpful for individuals over sixty years and those, with underlying health conditions that make invasive procedures risky.
It could be said that wireless pacemakers represent a progress in the field of cardiology technology. Through research and innovation upcoming versions of these devices might include functionalities like dual chamber pacing or improved integration with other cardiac monitoring tools. The possibilities offered by pacemakers have the potential to transform the management of different heart conditions enhancing patient care, reducing the invasiveness of procedures and increasing access to treatment, for patients worldwide.
At Felix Hospital, renowned cardiac specialists such as Dr. Rahul Arora, Dr. Syed Zafrul Hasan, and Dr. Siddharth Samrat are at the forefront of adopting and implementing such innovative technologies in cardiac care. Their expertise in cardiac surgery and the use of cutting-edge devices like wireless pacemakers ensures that patients receive the highest standard of care, with an emphasis on safety, effectiveness, and patient satisfaction.
Ready to explore the benefits of wireless pacemakers? Schedule a consultation with our expert cardiac team Contact us on 9667064100.
Wireless pacemakers have indeed proven to be a game changer for heart patients. Their ability to reduce complication risks, provide a minimally invasive treatment option, enhance patient comfort, and simplify follow-up care has made them an increasingly popular choice among both patients and healthcare providers. As technology continues to advance, the role of wireless pacemakers in cardiology is expected to expand, offering even greater benefits to patients suffering from heart rhythm disorders.
When considering this advanced treatment, it's important to understand the Pacemaker Surgery Cost in Noida. The cost can vary depending on factors such as the type of pacemaker, the expertise of the medical team, and the facilities offered by the hospital.
What is a wireless pacemaker?
A wireless pacemaker, or leadless pacemaker, is a small, self-contained device implanted directly into the heart via a catheter. Unlike traditional pacemakers, it does not require leads (wires) to connect to the heart, making it a more advanced and less invasive option.
How does a wireless pacemaker differ from a traditional pacemaker?
Traditional pacemakers use leads to transmit electrical signals from a pulse generator to the heart. In contrast, wireless pacemakers are entirely self-contained and implanted directly into the heart chamber, eliminating the need for leads and reducing complications.
What are the benefits of using a wireless pacemaker?
Wireless pacemakers offer several advantages, including reduced risk of complications related to leads, a minimally invasive implantation procedure, enhanced comfort and aesthetics, longer battery life, simplified follow-up care, and broader patient eligibility.
Are there any risks associated with wireless pacemakers?
While wireless pacemakers significantly reduce the risks associated with traditional pacemakers, potential risks may include device malfunction or migration. However, overall complication rates are lower due to the absence of leads and the minimally invasive procedure.
How is a wireless pacemaker implanted?
The implantation of a wireless pacemaker involves inserting a catheter through the femoral vein and placing the device directly into the right ventricle of the heart. This procedure is less invasive than traditional pacemaker surgeries and often allows for quicker recovery.
How long does the battery of a wireless pacemaker last?
The battery of a wireless pacemaker can last between 10 to 12 years, which is generally longer than the batteries of traditional pacemakers. The absence of leads contributes to the longer battery life.
Can wireless pacemakers be monitored remotely?
Yes, many wireless pacemakers feature remote monitoring capabilities, allowing healthcare providers to track the device's performance and the patient's heart rate without requiring frequent physical check-ups.
Who are the leading specialists for wireless pacemakers at Felix Hospital?
At Felix Hospital, renowned cardiac specialists like Dr. Rahul Arora, Dr. Syed Zafrul Hasan, and Dr. Siddharth Samrat are at the forefront of implementing and managing innovative technologies like wireless pacemakers. Their expertise ensures the highest standard of care for patients.
How can I schedule a consultation for a wireless pacemaker at Felix Hospital?
To explore the benefits of wireless pacemakers and receive expert advice, you can schedule a consultation with our cardiac specialists at Felix Hospital. Contact us today at 9667064100 to arrange an appointment and discuss your options.
हाइपरटेंशन जिसे उच्च रक्तचाप भी कहा जाता है। हाइपरटेंशन एक ऐसी स्थिति है जिसमें आपके रक्त का दबाव आपकी धमनियों की दीवारों पर बहुत अधिक होता है, जिससे पूरे शरीर में रक्त पंप करने, हृदय को अधिक काम करना पड़ता है। यह एक गंभीर स्वास्थ्य समस्या है। यह समय के साथ हृदय रोग, स्ट्रोक, और अन्य स्वास्थ्य संबंधी समस्याओं का कारण बन सकता है। अगर आपको हाइपरटेंशन तो तुरंत अच्छी चिकित्सीय सहायता प्राप्त करें। जानिए इसके लक्षण से लेकर इलाज तक के बारे में विस्तार से..
ज्यादा जानकारी के लिए हमें कॉल करें +91 9667064100.
रक्तचाप वह दबाव है जो रक्त आपके धमनियों की दीवारों पर डालता है जब यह हृदय द्वारा पंप किया जाता है। यह दो मुख्य घटकों से मिलकर बनता है। सिस्टोलिक दबाव और डायस्टोलिक दबाव। सिस्टोलिक दबाव तब होता है जब आपका हृदय धड़कता है और रक्त को धमनियों में पंप करता है। इसे रक्तचाप की माप में पहला (ऊपरी) संख्या द्वारा दर्शाया जाता है। डायस्टोलिक दबाव तब होता है जब हृदय की मांसपेशियां आराम करती हैं और यह दो धड़कनों के बीच का समय होता है। अगर आपका रक्तचाप 120/80 mmHg है, तो 120 mmHg सिस्टोलिक दबाव है और 80 mmHg डायस्टोलिक दबाव है। सामान्य रक्तचाप को 120/80 mmHg माना जाता है। इससे अधिक या कम रक्तचाप स्वास्थ्य समस्याओं का संकेत हो सकता है।
रक्तचाप के लक्षण अलग-अलग हो सकते हैं, और यह इस बात पर निर्भर करता है कि रक्तचाप उच्च (हाइपरटेंशन) है या निम्न (हाइपोटेंशन)।
हाइपरटेंशन को अक्सर "साइलेंट किलर" कहा जाता है क्योंकि इसके लक्षण सामान्यतः स्पष्ट नहीं होते, लेकिन कुछ लोगों में निम्नलिखित लक्षण हो सकते हैं:
निम्न रक्तचाप या हाइपोटेंशन के लक्षण आमतौर पर तब प्रकट होते हैं जब रक्तचाप बहुत कम हो जाता है:
अगर आपको इन लक्षणों का अनुभव हो रहा है, तो यह महत्वपूर्ण है कि आप चिकित्सा सलाह लें और अपने रक्तचाप की नियमित जांच कराएं।
रक्तचाप के मुख्य रूप से दो प्रकार होते हैं:
यह सबसे सामान्य प्रकार है और इसका कोई स्पष्ट कारण नहीं होता। यह उम्र, जीवनशैली, आहार और आनुवंशिक कारकों से विकसित हो सकता है।
यह किसी अन्य अंतर्निहित चिकित्सा स्थिति, जैसे किडनी रोग, हार्मोनल विकार या कुछ दवाओं के सेवन के कारण होता है। इस प्रकार का हाइपरटेंशन अक्सर अचानक प्रकट होता है और प्राथमिक हाइपरटेंशन की तुलना में अधिक गंभीर होता है।
अलग अलग परिस्थितियों के कारण हो सकते हैं।
यह तब होता है जब आप अचानक बैठने या लेटने की स्थिति से खड़े होते हैं, जिससे चक्कर आना या बेहोशी हो सकती है। यह सामान्य रूप से वृद्ध व्यक्तियों में देखा जाता है।
यह लंबे समय तक खड़े रहने के बाद होता है और विशेष रूप से बच्चों और युवा वयस्कों में देखा जाता है।
यह तब होता है जब रक्तचाप इतना कम हो जाता है कि शरीर के महत्वपूर्ण अंगों को पर्याप्त रक्त की आपूर्ति नहीं होती। यह शॉक के कारण हो सकता है और जीवन के लिए खतरा बन सकता है।
इनके अलावा रक्तचाप के अन्य प्रकार भी हो सकते हैं, जैसे कि इमरजेंसी हाइपरटेंशन, जो अचानक और अत्यधिक रक्तचाप में वृद्धि होती है और इसे तुरंत चिकित्सा देखभाल की आवश्यकता होती है।
रक्तचाप के बढ़ने या घटने के कई कारण हो सकते हैं। ये कारण व्यक्ति की जीवनशैली, आहार, आनुवंशिकता, और अन्य स्वास्थ्य स्थितियों पर निर्भर करते हैं।
अनियमित खानपान:
अधिक नमक और फैट का सेवन और कम फल-सब्जियों का सेवन रक्तचाप को बढ़ा सकता है।
मोटापा:
अधिक वजन हृदय पर दबाव डालता है, जिससे रक्तचाप बढ़ सकता है।
शारीरिक निष्क्रियता:
नियमित व्यायाम की कमी से रक्तचाप बढ़ने का खतरा होता है।
धूम्रपान और शराब:
धूम्रपान और अत्यधिक शराब का सेवन रक्तचाप को बढ़ा सकता है।
तनाव:
लगातार तनाव में रहने से रक्तचाप में वृद्धि हो सकती है।
आनुवंशिकता:
अगर परिवार में उच्च रक्तचाप का अनुवांशिक इतिहास है, तो इसका खतरा अधिक हो सकता है।
पुरानी बीमारियां:
मधुमेह, किडनी की बीमारी और कुछ हार्मोनल विकार उच्च रक्तचाप के कारण हो सकते हैं।
उम्र:
उम्र बढ़ने के साथ रक्तचाप बढ़ने की संभावना अधिक होती है।
दवाइयां:
कुछ दवाइयों के साइड इफेक्ट के रूप में रक्तचाप बढ़ सकता है।
रक्तचाप के नियंत्रण के लिए इन कारणों की पहचान और उनका प्रबंधन महत्वपूर्ण है। यदि रक्तचाप से संबंधित कोई समस्या हो, तो डॉक्टर से परामर्श अवश्य करना चाहिए।
रक्तचाप को नियंत्रित और स्वस्थ रखने के लिए कुछ महत्वपूर्ण उपाय किए जा सकते हैं। इन उपायों को अपनाकर आप उच्च या निम्न रक्तचाप से बच सकते हैं:
स्वस्थ आहार:
कम नमक, संतृप्त वसा और चीनी का सेवन करें। फलों, सब्जियों, साबुत अनाज और कम वसा वाले डेयरी उत्पादों का सेवन बढ़ाएं। पोटेशियम से भरपूर आहार (जैसे केले, संतरे, पालक) लें, जो रक्तचाप को नियंत्रित करने में मदद करता है।
नियमित व्यायाम:
सप्ताह में कम से कम 150 मिनट की मध्यम-तीव्रता की शारीरिक गतिविधि (जैसे चलना, तैराकी, साइकलिंग) करें। नियमित व्यायाम से वजन नियंत्रित रहता है और दिल की सेहत में सुधार होता है।
वजन प्रबंधन:
स्वस्थ वजन बनाए रखें। अतिरिक्त वजन घटाने से रक्तचाप कम करने में मदद मिलती है।
धूम्रपान और शराब से बचें:
धूम्रपान छोड़ें और शराब का सेवन सीमित करें। धूम्रपान से धमनियां संकरी हो जाती हैं, जिससे रक्तचाप बढ़ सकता है।
तनाव प्रबंधन:
योग, ध्यान और गहरी सांस लेने के व्यायाम से तनाव को कम करें। समय-समय पर आराम करें और अपने मनपसंद कार्यों में शामिल हों।
नियमित जांच:
नियमित रूप से रक्तचाप की जांच कराएं, खासकर अगर आप जोखिम में हैं। अगर आपका रक्तचाप सामान्य से अधिक है, तो डॉक्टर के परामर्श के अनुसार दवा लें।
पर्याप्त पानी पिएं:
शरीर में पानी की कमी न होने दें।निर्जलीकरण से रक्तचाप कम हो सकता है। ज्यादा पसीना आने या गर्मी में अधिक मात्रा में पानी का सेवन करें।
संतुलित आहार लें:
भोजन में संतुलन बनाए रखें और आवश्यक पोषक तत्वों का सेवन करें। ज्यादा समय तक भूखे न रहें और छोटे-छोटे अंतराल पर भोजन करें।
कैफीन का सेवन करें:
कैफीन युक्त पेय जैसे चाय या कॉफी का सीमित मात्रा में सेवन करने से रक्तचाप को थोड़ा बढ़ाने में मदद मिल सकती है, लेकिन इसका अत्यधिक सेवन नहीं करना चाहिए।
धीरे-धीरे उठें:
लेटे या बैठे हुए स्थिति से धीरे-धीरे खड़े हों। अचानक उठने से चक्कर आ सकते हैं और रक्तचाप कम हो सकता है।
नमक का सेवन डॉक्टर की सलाह पर करें:
अगर आपका रक्तचाप सामान्य से कम है, तो डॉक्टर के परामर्श अनुसार अपने आहार में थोड़ा अधिक नमक शामिल कर सकते हैं।
सही मोजे पहनें:
सही मोजे पहनने से पैरों में खून जमा नहीं होता, जिससे रक्तचाप में कमी आती है।
इन उपायों को अपनाकर रक्तचाप को नियंत्रित रखा जा सकता है और इसके कारण होने वाली स्वास्थ्य समस्याओं से बचा जा सकता है।
रक्तचाप का इलाज इस बात पर निर्भर करता है कि रक्तचाप उच्च (हाइपरटेंशन) है या निम्न (हाइपोटेंशन)। यहाँ दोनों स्थितियों के लिए उपयुक्त उपचार दिए गए हैं:
जीवनशैली में बदलाव:
नमक का सेवन कम करें। फलों, सब्जियों, साबुत अनाज, और कम वसा वाले डेयरी उत्पादों का सेवन बढ़ाएं।
नियमित व्यायाम:
प्रतिदिन 30 मिनट मध्यम-तीव्रता वाली शारीरिक गतिविधि जैसे तेज चलना, साइक्लिंग या तैराकी करें।
वजन प्रबंधन:
स्वस्थ वजन बनाए रखें, क्योंकि वजन कम करने से रक्तचाप कम हो सकता है।
धूम्रपान और शराब से परहेज:
धूम्रपान छोड़ें और शराब का सेवन सीमित करें।
तनाव प्रबंधन:
योग, ध्यान और गहरी सांस लेने के अभ्यास करें।
दवाइयां:
डायूरेटिक्सः
जिनके शरीर से अतिरिक्त सोडियम और पानी निकालते हैं, जिससे रक्तचाप कम होता है।
बीटा-ब्लॉकर्स :
हृदय की धड़कन को धीमा करते हैं और रक्तचाप को कम करते हैं।
एस इनहिबिटर :
धमनियों को संकुचित होने से रोकते हैं।
कैल्शियम चैनल ब्लॉकर्स :
धमनियों को चौड़ा करते हैं और हृदय की धड़कन को धीमा करते हैं।
एंजियोटेंसिन II रिसेप्टर ब्लॉकर्स:
धमनियों को चौड़ा करने में मदद करते हैं।
जीवनशैली में सुधार:
निर्जलीकरण से बचने के लिए पानी का अधिक सेवन करें। डॉक्टर के परामर्श से आहार में नमक की मात्रा बढ़ाएं। सीमित मात्रा में कैफीन युक्त पेय (जैसे चाय, कॉफी) लें। धीरे-धीरे उठें: लेटने या बैठने से खड़े होते समय धीरे-धीरे उठें। छोटे और बार-बार भोजन: अर्थात छोटे अंतराल पर भोजन करें।
फ्लूड्रोकोर्टिसोन :
रक्त में सोडियम की मात्रा बढ़ाकर रक्तचाप को नियंत्रित करता है।
मिडोड्राइन :
धमनियों को संकुचित कर रक्तचाप बढ़ाता है।
सही मोजे पहने:
पैरों में रक्त के संचलन में सुधार के लिए संपीड़न मोजे पहनें।
यदि आपको रक्तचाप से संबंधित कोई समस्या हो तो डॉक्टर से परामर्श अवश्य करें। आपकी स्थिति के आधार पर सही इलाज और दवाइयों का निर्धारण किया जाएगा।
हाइपरटेंशन का इलाज मुख्य रूप से जनरल फिजिशियन या इंटर्नल मेडिसिन विशेषज्ञ करते हैं। फेलिक्स हॉस्पिटल में हाइपरटेंशन ट्रीटमेंट एक्सपर्ट डॉ. अंशुमाला सिन्हा, डॉ. सोनाक्षी सक्सेना, और डॉ. प्रियंका सिंह आदि हैं। ये डॉक्टर रक्तचाप की नियमित निगरानी, जीवनशैली में बदलाव, और आवश्यक दवाओं का प्रबंधन कर सकते हैं। अगर हाइपरटेंशन से हृदय संबंधी समस्याएं पैदा हो रही हों तो कार्डियोलॉजिस्ट उपचार में शामिल होते हैं। अगर हाइपरटेंशन किडनी की समस्याओं से संबंधित हो, तो नेफ्रोलॉजिस्ट इसका इलाज करते हैं। अगर हाइपरटेंशन का कारण हार्मोनल असंतुलन हो, तो एंडोक्रिनोलॉजिस्ट इसका इलाज कर सकते हैं।
हाइपरटेंशन का इलाज मुख्य रूप से जनरल फिजिशियन या इंटर्नल मेडिसिन विशेषज्ञ करते हैं। ये डॉक्टर रक्तचाप की नियमित निगरानी, जीवनशैली में बदलाव, और आवश्यक दवाओं का प्रबंधन कर सकते हैं। अगर हाइपरटेंशन से हृदय संबंधी समस्याएं पैदा हो रही हों तो कार्डियोलॉजिस्ट उपचार में शामिल होते हैं। अगर हाइपरटेंशन किडनी की समस्याओं से संबंधित हो, तो नेफ्रोलॉजिस्ट इसका इलाज करते हैं। अगर हाइपरटेंशन का कारण हार्मोनल असंतुलन हो, तो एंडोक्रिनोलॉजिस्ट इसका इलाज कर सकते हैं। डॉक्टर की सलाह के लिए आज ही फ़ोन करें - +91 9667064100.
हाइपरटेंशन एक प्रमुख सार्वजनिक स्वास्थ्य मुद्दा है, जो दुनिया भर में बड़ी संख्या में लोगों को प्रभावित करता है और विभिन्न जीवनशैली से जुड़ी बीमारियों के जोखिम को बढ़ाता है। हाइपरटेंशन के बारे में जागरूकता बढ़ाना और स्वास्थ्य शिक्षा प्रदान करना आवश्यक है, ताकि लोग इस स्थिति की पहचान और प्रबंधन के बारे में जान सकें और उचित कदम उठा सकें। हाइपरटेंशन का सही और समय पर प्रबंधन आपके स्वास्थ्य को बेहतर बना सकता है और दीर्घकालिक स्वास्थ्य समस्याओं के जोखिम को कम कर सकता है।
प्रश्न 1: हाइपरटेंशन का क्या कारण है ?
उत्तर: हाइपरटेंशन के कई कारण हो सकते हैं, जिनमें अनियमित खानपान, मोटापा, धूम्रपान, शराब का सेवन, तनाव और आनुवांशिक कारण शामिल हैं।
प्रश्न 2: हाइपरटेंशन की जांच कैसे की जाती है ?
उत्तर: हाइपरटेंशन की जांच करने के लिए एक साधारण ब्लड प्रेशर मापने वाला उपकरण इस्तेमाल किया जाता है। सामान्य रक्तचाप 120/80 mmHg होता है। अगर यह 140/90 mmHg या इससे अधिक हो, तो यह हाइपरटेंशन माना जाता है।
प्रश्न 3: हाइपरटेंशन का इलाज कैसे किया जाता है ?
उत्तर: हाइपरटेंशन का इलाज जीवनशैली में बदलाव और दवाओं के माध्यम से किया जा सकता है। इसमें नियमित व्यायाम, संतुलित आहार, कम नमक का सेवन, धूम्रपान और शराब से बचाव शामिल हैं। कुछ मामलों में डॉक्टर दवाएं भी लिख सकते हैं।
प्रश्न 4: क्या हाइपरटेंशन को रोका जा सकता है ?
उत्तर: हां, हाइपरटेंशन को स्वस्थ जीवनशैली अपनाकर रोका जा सकता है। इसमें सही आहार, नियमित व्यायाम, वजन नियंत्रित रखना, और तनाव को प्रबंधित करना शामिल है।
प्रश्न 5: हाइपरटेंशन के दीर्घकालिक प्रभाव क्या हैं ?
उत्तर: अगर हाइपरटेंशन का सही समय पर इलाज नहीं किया जाए, तो इससे हृदय रोग, किडनी की समस्याएं, स्ट्रोक और आंखों की समस्याएं हो सकती हैं।
प्रश्न 6: क्या हाइपरटेंशन एक जीवनभर की समस्या है ?
उत्तर: हाइपरटेंशन को नियंत्रित किया जा सकता है, लेकिन इसे पूरी तरह से ठीक करना मुश्किल हो सकता है। इसलिए, इसे जीवनभर प्रबंधित करना आवश्यक होता है।
प्रश्न 7: क्या हाइपरटेंशन के लिए नियमित जांच आवश्यक है ?
उत्तर: हां, अगर आपको हाइपरटेंशन है, तो आपके लिए नियमित रूप से ब्लड प्रेशर की जांच कराना जरूरी है ताकि इसे नियंत्रण में रखा जा सके।
प्रश्न 8 : हाइपरटेंशन के जोखिम को कैसे कम किया जा सकता है ?
उत्तर: जोखिम को कम करने के लिए धूम्रपान और शराब का सेवन छोड़ें, स्वस्थ आहार लें, नियमित व्यायाम करें, और तनाव को प्रबंधित करने की कोशिश करें।

Heart attacks and strokes are both serious medical emergencies that can have devastating effects on health and well-being. Despite their similarities, they are distinct conditions with different causes, symptoms, and treatments. Understanding the differences between them is crucial for recognising symptoms early and seeking appropriate care. Here’s a closer look at how heart attacks and strokes differ, including the important distinction in strokes and heart attacks symptoms and what you need to know about each.
Contact Felix Hospital in Noida for expert emergency care and consultations with our leading specialists. Call now at 9667064100.
A heart attack, or myocardial infarction,occurs when the blood supply to a portion of the heart is cut off due to the formation of a blood clot in one of the coronary arteries. The critical issue with this disease is that when the heart muscle fails to receive adequate oxygenated blood, it begins to die, potentially leading to significant damage. To ensure the best outcomes, seeking treatment from the best heart attack surgeon is crucial for effective management and recovery.
Atherosclerosis: The primary risk factor for a heart attack or an acute myocardial infarction is atherosclerosis, or the deposit of fatty substances in the coronary arteries. They accumulate gradually in the arteries, and over time, they constrict the arteries, thus increasing the tendency to thrombosis formation.
Blood Clots: An occlusion of the blood vessels supplying the heart muscle can result from the formation of a blood clot in the coronary arteries.
Spasms: Occasionally the arteries supplying the heart, known as the coronary arteries, constrict and may completely occlude the blood supply to the heart for short periods of time.
Heart attack symptoms can vary but typically include:
It's crucial to recognise these signs, as heart attacks can be dangerous and even fatal if not treated promptly.
Immediate treatment for a heart attack usually involves:
A stroke occurs when the blood supply to a specific area in the brain is reduced or completely stopped, necessitating the lack or minimal supply of both oxygen and nutrients to the brain cells. This interruption can lead to brain damage and serious complications. Strokes are classified into two main types: the ischaemic and the hemorrhagic stroke.
Symptoms of stroke can appear suddenly and may include:
Immediate treatment for a stroke depends on the type and includes:
1-Origin of the Problem
2. Cause
3. Symptoms
Heart Attack
Heart attack signs could arise unexpectedly. Develop gradually over a span of hours (or possibly even days). The typical indications of a heart attack encompass;
1-Symptoms of stroke can include:
2-Stroke often affects a person’s face, arms, and speech.
3-Treatment Approaches
May involve both clot-dissolving drugs and surgical interventions depending on the type of stroke.
4-Prevention:
Dr. Syed Zafrul Hasan
Dr. Syed Zafrul Hasan, MBBS, PGDCC, ACMDC, BLS, ACLS, is a seasoned Interventional Cardiologist with over 13 years of experience. His expertise encompasses both non-invasive procedures, such as ECHO, DSE Stress Echo, and TMT, as well as invasive techniques, including TPI, central line insertion, arterial line insertion, and intubation. Dr. Hasan is well-equipped to address a wide range of cardiac and chronic conditions, including hypertension, diabetes, elevated cholesterol, heart attacks, and peripheral vascular disease.
Dr. Siddharth Samrat
Dr. Siddharth Samrat, MBBS, MD, DM, is a proficient Cardiologist with two years of experience. He has performed over 500 coronary angiographies, 250+ angioplasties, and 150+ pacemaker implantations. His skills extend to a range of procedures including angioplasty, pacemaker insertion, CRT-D/P, PTMC for mitral stenosis, and device closures. Specializing in complex coronary interventions, coronary imaging, and congenital heart disease, he also treats chronic conditions like hypertension, diabetes, and elevated cholesterol.
Schedule your appointment now to receive personalized care and expert advice tailored to your needs. Contact us today at 9667064100.
Ultimately even though Heart Attacks and strokes exhibit similarities they represent unique health issues with varying origins, therapies and indications. Grasping these distinctions is vital for identifying the need for attention promptly as early action plays a crucial role in managing the conditions effectively. Furthermore, having knowledge about the Cost to treating heart attacks can aid in preparing for efficient medical care.
In case of an emergency situation where you notice signs of a heart attack or stroke it's crucial to seek medical help. Taking steps for your health is essential especially as early intervention can greatly enhance recovery prospects.

Recent studies show that cardiovascular diseases are the leading cause of death among women, accounting for 1 in 4 female deaths globally. In India, particularly within urban areas, the prevalence of heart disease has been rising. Alongside common risk factors such as stress, hypertension, diabetes, and obesity, there are also gender-specific risk factors that elevate the risk of heart disease in women. For those in Noida, timely and effective Heart Attack Treatment in Noida is crucial for managing this serious condition. Recognizing the early signs, understanding the symptoms, and knowing the different types of heart diseases are crucial for effective prevention and management.
Don’t wait to take charge of your heart health. Contact Felix Hospital in Noida for effective heart attack treatment. Schedule a comprehensive heart health check-up today. Call Now 9667064100.
Heart disease, or cardiovascular disease, encompasses a range of conditions affecting the heart. Here are some common types of heart diseases in women:
In addition to diabetes and unhealthy habits like smoking or high blood pressure and cholesterol levels that are known risk factors for heart disease in both men and women; there are risk factors that are unique to women.
It is essential to be vigilant in identifying symptoms of Heart Diseases in Women since they may exhibit unconventional signs that could hinder timely diagnosis unlike their male counterparts who typically display more obvious signs of heart disease.
Knowing about these signs can assist in getting help promptly and enhancing the outcomes of heart health.
Adopting a heart-healthy lifestyle is crucial in preventing heart disease. This includes
1-Healthy Lifestyle Choices
2-Routine Health Check-ups
Regular health check-ups are essential in detecting risk factors for heart disease early. Keeping track of blood pressure levels and checking cholesterol and blood sugar regularly can help pinpoint issues before they worsen significantly.
Moreover women who have a family history of heart disease or other risk factors should have a conversation about their risk with their healthcare provider. Adhere to the suggested screening guidelines.
Dealing with long term stress can harm the hearts well being. Coming to grips with stress through practices like mindfulness exercises or yoga as well as seeking counseling can minimize its effects on the body. It's vital to discover strategies to handle stress and prioritize relaxation and self care time.
Smoking poses a threat to heart health and is especially harmful to women's hearts as well as men's hearts too. Stopping smoking can greatly lower the chances of developing heart disease. With binge drinking. It can raise blood pressure and lead to heart issues; hence it's crucial to consume alcohol in moderation.
Women with illnesses like diabetes or hypertension must focus on effectively managing these conditions to safeguard their heart health. By adhering to prescribed medications and dietary guidelines while making necessary lifestyle adjustments can help in controlling the condition.
Reach out today to consult with our specialists and take the first step towards a healthier heart. Call us at 9667064100.
Understanding heart disease and its risk factors empowers women to take charge of their health. However, it’s also important to seek help and support from healthcare professionals. Regular consultations with a doctor can provide personalized advice and ensure that any potential issues are addressed promptly.
Women should also consider joining support groups or programs focused on heart health, as they can provide valuable information, resources, and a sense of community. This support can be especially beneficial in addressing coronary heart disease risk factors for women, offering motivation and encouragement to manage and reduce those risks effectively.
Dr. Rahul Arora, MBBS, MD, DM (Cardiology)
With over 13 years of experience, Dr. Rahul Arora specializes in minimal access cardiac surgery (MICS), showcasing his innovative approach and dedication to advanced cardiology.
Dr. Syed Zafrul Hasan, MBBS, PGDCC, ACMDC, BLS, ACLS
Dr. Syed Zafrul Hasan brings more than 13 years of experience in both non-invasive procedures (ECHO, stress ECHO, TMT) and invasive techniques (TPI, central and artery line insertion, intubation), offering a comprehensive approach to cardiac care.
Dr. Siddharth Samrat, MBBS, MD, DM (Cardiology)
Specializing in minimally invasive cardiac procedures, Dr. Siddharth Samrat has performed over 500 coronary angiograms and 250+ angioplasties, alongside numerous pacemaker implantations, demonstrating his expertise in advanced cardiac interventions.
Our Best Heart Surgeons in Noida are dedicated to providing exceptional heart care with their extensive experience and innovative techniques.
Heart disease is a significant concern for women, but with awareness and proactive measures, it is possible to reduce the risk and lead a heart-healthy life. By understanding the unique risks, making healthy lifestyle choices, managing chronic conditions, and seeking regular medical care, women can protect their heart health and improve their overall well-being. Prioritizing these measures enhances overall health and mitigates the risk of heart disease in women.
If you have any concerns about your heart health or risk factors for heart disease, don’t hesitate to reach out to a healthcare provider. Early intervention and a commitment to a heart-healthy lifestyle can make all the difference in maintaining a healthy heart for years to come.
1-What are the main factors that increase the risk of heart disease in women?
ANS: Common risk factors consist of hypertension, elevated cholesterol levels, diabetes, obesity, smoking, excessive alcohol intake and leading a lifestyle. Women face risks related to menopause and pregnancy like preeclampsia and autoimmune illnesses such as lupus and rheumatoid arthritis.
2-How does menopause impact the chances of heart disease in women?
ANS: After menopause occurs in women's bodies, the natural decrease in estrogen levels takes place. This leads to a chance of heart disease due to the loss of its protective effects on the heart. The combination of this factor with other risks leads to an increased susceptibility to heart issues for postmenopausal women.
3-How frequently should women have their heart health assessed?
ANS: It's important for women to get health check ups that cover blood pressure checks and tests, for cholesterol levels and blood sugar levels regularly based on their individual risk factors and overall health condition; although it's generally advised to have annual check ups as a standard practice.
4-Is it possible for women with illnesses to lower their chances of developing heart disease?
ANS: Certainly! By handling long term conditions like diabetes or hypertension through dedicated adherence to treatment plans and a healthy lifestyle, alongside regular medical check ups can notably lower the likelihood of developing heart disease.
5-How does stress affect the heart health of women?
ANS: Chronic stress can have an impact on heart health by leading to elevated blood pressure levels and promoting unhealthy dietary choices that increase the likelihood of heart disease development. Those dealing with stress can find relief through practices such as yoga sessions and meditation. Seek support from therapy to reduce these harmful effects on the heart.
6-How does a woman's family history impact her chances of developing heart disease?
ANS: If a woman has a family history of heart disease her chances of developing issues may be higher so she should pay close attention to her heart health and consider starting preventive measures or screenings earlier than usual.
Heart disease is often thought of as a condition that primarily affects men, but the truth is, women are also at significant risk. In fact, heart disease is the leading cause of death for women worldwide. Understanding the risks and taking steps for prevention can make a huge difference in women’s health outcomes. Here’s a closer look at why heart disease is such a critical issue for women and how they can take control of their heart health.
1-Healthy Lifestyle Choices
Adopting a heart-healthy lifestyle is crucial in preventing heart disease. This includes:
2-Regular Health Screenings
Regular health check-ups are essential in detecting risk factors for heart disease early. Women should have their blood pressure, cholesterol levels, and blood glucose levels checked regularly. These screenings can help identify potential problems before they become more serious.
Additionally, women with a family history of heart disease or other risk factors should discuss their risk with their healthcare provider and follow recommended screening guidelines.
3-Managing Stress
Chronic stress can have a negative impact on heart health. Learning to manage stress through techniques such as mindfulness, meditation, yoga, or counseling can help reduce its impact on the body. It’s important to find healthy ways to cope with stress and make time for relaxation and self-care.
4-Avoiding Tobacco and Limiting Alcohol
Smoking is a major risk factor for heart disease and has a particularly detrimental effect on women’s heart health. Quitting smoking can significantly reduce the risk of heart disease. Similarly, excessive alcohol consumption can increase blood pressure and contribute to heart problems, so it’s important to drink in moderation.
5-Managing Chronic Conditions
For women with chronic conditions such as diabetes or high blood pressure, managing these conditions effectively is crucial for heart health. This may involve taking prescribed medications, following a special diet, and making lifestyle changes to keep the condition under control.
Seeking Help and Support
Understanding heart disease and its risk factors empowers women to take charge of their health. However, it’s also important to seek help and support from healthcare professionals. Regular consultations with a doctor can provide personalized advice and ensure that any potential issues are addressed promptly.
Women should also consider joining support groups or programs focused on heart health. These can offer valuable information, resources, and a sense of community that can be motivating and encouraging.
Heart disease is a significant concern for women, but with awareness and proactive measures, it is possible to reduce the risk and lead a heart-healthy life. By understanding the unique risks, making healthy lifestyle choices, managing chronic conditions, and seeking regular medical care, women can protect their heart health and improve their overall well-being.
If you have any concerns about your heart health or risk factors for heart disease, don’t hesitate to reach out to a healthcare provider. Early intervention and a commitment to a heart-healthy lifestyle can make all the difference in maintaining a healthy heart for years to come.

In today’s fast-paced world, where stress is our constant companion,it's easy to overlook the well-being of our most vital organ - the heart. However, maintaining heart health is crucial and doesn't have to be as complicated as you might think. This guide introduces Life's Simple Seven, a straightforward yet effective approach to heart health that can significantly improve your overall well-being. Whether you're in your vibrant twenties or your golden fifties, it's never too early or too late to start prioritizing your heart health.
Unlock the secrets to a healthier heart. Click here or call +91 9667064100 to get started!
Physical activity is a cornerstone of heart health. It helps control weight, reduces the risk of cardiovascular disease, and reduces stress levels. Additionally, regular exercise improves circulation and boosts overall energy, contributing to a healthier, more vibrant life.
How can you incorporate more movement into your life?
A nutritious diet is crucial for a strong cardiovascular system. It helps regulate blood pressure, maintain healthy cholesterol levels, and support overall heart function. Additionally, incorporating a variety of nutrient-rich foods can enhance circulation, reduce inflammation, and improve heart health, contributing to a more robust and resilient cardiovascular system.
What constitutes a heart-healthy diet?
Excess weight puts extra strain on your heart, increases blood pressure, and raises the risk of type 2 diabetes. It can also lead to higher cholesterol levels and contribute to cardiovascular disease, making weight management essential for long-term health and well-being.
How to achieve and maintain a healthy weight?
Cholesterol is essential for your body, but an excess of the wrong type can lead to heart disease. Elevated levels of LDL (bad cholesterol) can cause plaque buildup in the arteries, increasing the risk of heart attack and stroke. Maintaining a healthy cholesterol balance through diet and lifestyle is vital for cardiovascular health. For comprehensive care and guidance on managing cholesterol and heart health, consider visiting the best heart hospital in Noida.
What you need to know?
How to manage your cholesterol:
Get regular check-ups: Know your numbers and work with your healthcare provider to interpret them.
High blood pressure, often called the "silent killer," can damage your heart and blood vessels without obvious symptoms. Over time, it increases the risk of heart disease, stroke, and kidney damage, making regular monitoring and management essential for long-term health.
How to keep it in check?
High blood sugar can damage blood vessels and nerves that control your Heart. This damage increases the risk of cardiovascular complications, including heart disease and stroke. Persistent high blood sugar can also lead to poor circulation and contribute to long-term health issues if not properly managed through lifestyle changes and medication.
How to maintain healthy blood sugar levels?
Quitting smoking is one of the best things you can do for your heart health. It helps lower your risk of heart disease, improves circulation, and reduces blood pressure. Additionally, giving up smoking enhances overall cardiovascular health and supports long-term well-being, leading to a healthier, longer life.
Why and how to quit smoking?
Understand the risks: Smoking damages blood vessels, reduces blood oxygen, and increases heart disease risk.
Know the benefits of quitting: Your body begins to heal as soon as you quit, with significant improvements in heart disease risk within one year.
Dr. Rahul Arora
Dr. Rahul Arora, MBBS, MD, DM, is considered one of the best heart specialists in Noida, with over 13 years of experience in interventional cardiology. Renowned for his exceptional patient care and innovative techniques, Dr. Arora excels in maintaining optimal heart health and managing cardiovascular conditions.
Dr. Siddharth Samrat
Dr. Siddharth Samrat, MBBS, MD, DM, stands out as a top heart specialist in Noida with two years of focused experience in heart health. Having performed over 500 angiographies and 250+ angioplasties, Dr. Samrat is a leading choice for complex coronary interventions and managing chronic heart issues.
Dr. Syed Zafrul Hasan
Dr. Syed Zafrul Hasan, MBBS, PGDCC, ACMDC, BLS, ACLS, is a leading heart specialist in Noida with 13 years of expertise. Skilled in both non-invasive and invasive cardiology procedures, Dr. Hasan is dedicated to managing and maintaining heart health, including conditions like hypertension and diabetes.
Implementing these seven principles can greatly enhance your heart health and overall quality of life. Start with small, manageable changes and gradually build healthier habits. Every positive step you take contributes to better cardiovascular health and a higher quality of life. For those seeking support, consulting healthcare professionals is crucial as they can offer personalized advice and help you navigate your heart health journey. If you're also looking for the Best heart treatment cost in Noida, professional guidance can ensure you receive the best value for top-quality care.
Ready to transform your heart health? Call +91 9667064100 to get started!
1. What are the signs of a healthy heart?
Signs of a healthy heart include normal blood pressure, a steady and regular heartbeat, good circulation, and the absence of chest pain or discomfort. Additionally, healthy cholesterol levels and consistent energy levels throughout the day indicate that your heart is functioning well.
2.What foods are good for the heart?
Foods beneficial for heart health include fruits, vegetables, whole grains, and fatty fish rich in omega-3 fatty acids. Nuts, seeds, legumes, and foods high in fiber, such as oats and beans, also support heart health by improving cholesterol levels and reducing inflammation.
3.How to increase heart strength?
To increase heart strength, engage in regular cardiovascular exercises such as brisk walking, running, or cycling. Incorporate strength training and interval training into your routine. Additionally, maintain a balanced diet, manage stress, stay hydrated, and avoid smoking to support overall cardiovascular health.
4.Which exercise is best for the heart?
Aerobic exercises, such as running, swimming, or cycling, are best for heart health. These activities improve cardiovascular endurance, increase heart efficiency, and help manage weight. Incorporating moderate to vigorous intensity workouts several times a week can significantly enhance heart strength and overall fitness.
5.How much walking is healthy for your heart?
Walking for at least 150 minutes a week, or about 30 minutes on most days, is healthy for your heart. This moderate-intensity exercise helps improve cardiovascular health, manage weight, and reduce the risk of heart disease. Consistent walking can enhance overall well-being and boost heart function.

Recognizing heart attack signs early is crucial because timely intervention can significantly reduce the risk of severe complications and improve outcomes. Early detection allows for prompt medical treatment, which can restore blood flow to the heart and minimize damage to the heart muscle. Therefore, being aware of the symptoms and acting quickly by seeking emergency medical help from the best heart attack surgeon in Noida can be life-saving and is essential for effective heart attack management. Understanding why a heart attack occurs is also important, as it can help in identifying risk factors and implementing preventive measures.
Recognize the signs and act quickly! Call +91 9667064100 or click here for immediate assistance.
A heart attack, or myocardial infarction, occurs when blood flow to a part of the heart is blocked, usually by a blood clot forming in a coronary artery that has been narrowed by plaque buildup. This blockage deprives the heart muscle of oxygen, leading to damage or death of the heart tissue. Several risk factors contribute to heart attacks, including high blood pressure, high cholesterol, smoking, obesity, diabetes, and a sedentary lifestyle. Stress and a family history of heart disease also play significant roles in increasing an individual’s risk.
Recognizing the warning signs of a heart attack is crucial for timely intervention. While chest pain is the most commonly associated symptom, heart attacks can present in various ways.
Chest discomfort is frequently described as pressure, squeezing, fullness, or pain in the center or left side of the chest. This sensation can last for several minutes or intermittently come and go. It’s important to recognize that this discomfort might not always be intense; sometimes it may feel like mild pressure or heaviness.
The discomfort associated with a Heart Attack often radiates to other parts of the body. Common areas include the shoulders, arms, back, neck, jaw, or stomach. Women, in particular, may experience less typical symptoms, such as pain or discomfort that radiates to different areas than those usually associated with heart attacks.
Shortness of breath can occur with or without accompanying chest discomfort. This symptom might feel like a sudden inability to catch one’s breath or a sense of breathlessness. It can be a crucial indicator of a heart attack, especially when it occurs suddenly or unexpectedly.
Experiencing cold sweats, feeling nauseous, or having lightheadedness are also possible warning signs of a heart attack. These symptoms may accompany chest discomfort or occur independently, signaling that immediate medical attention is needed.
Unusual or unexplained fatigue, particularly in the days or weeks leading up to a heart attack, can be an early warning sign. This fatigue might be accompanied by sleep disturbances and may be more pronounced in women.
Heart palpitations or an awareness of an irregular heartbeat can also indicate potential cardiac issues. These palpitations may be accompanied by other symptoms or occur on their own, warranting further investigation to rule out or address underlying heart conditions.
If you experience any symptoms indicative of a heart attack, such as chest pain, shortness of breath, or radiating discomfort, it's crucial to seek immediate medical attention. Visiting the best heart attack hospital in Noida will ensure that you receive the highest standard of care. These specialized facilities are equipped with advanced diagnostic tools, experienced cardiologists, and comprehensive treatment options to address heart attacks effectively. Prompt intervention can significantly improve outcomes and reduce the risk of severe complications.
Dr. Rahul Arora, MBBS, MD, DM (Cardiology), is a highly experienced Interventional Cardiologist with over 13 years of expertise in managing heart attacks. His extensive background in advanced interventional techniques allows him to provide swift and effective treatment during acute cardiac events. Dr. Arora excels in using cutting-edge technology for coronary interventions, including angioplasty and stenting, to restore blood flow and improve patient outcomes in critical situations.
Dr. Syed Zafrul Hasan, MBBS, PGDCC, ACMDC, BLS, ACLS, has over 13 years of experience as an Interventional Cardiologist specializing in the treatment of heart attacks. His comprehensive approach includes both Non-Invasive assessments like ECHO and TMT and crucial Invasive interventions such as arterial line insertion and temporary pacemaker placement. Dr. Hasan's broad skill set ensures precise and timely management of heart attacks, addressing urgent and complex cardiac conditions effectively.
Dr. Siddharth Samrat, MBBS, MD, DM (Cardiology), is a proficient Cardiologist with two years of focused experience in heart attack treatment. In this period, he has performed over 500 coronary angiographies and 250+ angioplasties, demonstrating his expertise in rapidly addressing acute coronary events. Dr. Samrat’s proficiency in advanced interventional techniques ensures effective and timely treatment, helping to improve patient recovery and outcomes during heart attacks.
Recognizing the warning signs of a heart attack is crucial for timely intervention and treatment. Symptoms such as chest discomfort, shortness of breath, pain radiating to other parts of the body, cold sweats, nausea, unexplained fatigue, and heart palpitations should not be ignored. These signs often indicate that the heart is not receiving enough oxygen and requires immediate medical attention. If you or someone you know exhibits any of these symptoms, especially if they persist or worsen, it is essential to seek emergency medical help without delay. Additionally, staying informed about heart health and understanding the Heart Attack Surgery Treatment Cost in Noida can help you make better decisions in critical situations and ensure the best possible care.
For further inquiries or assistance, simply click here or contact us at +91 9667064100.
1. How do you know you're having a heart attack?
Symptoms of a Heart Attack can include chest discomfort, pain radiating to the shoulders, arms, neck, or jaw, shortness of breath, nausea, cold sweats, and unexplained fatigue. Immediate medical evaluation is crucial if these symptoms occur.
2. What should I do if I experience heart attack symptoms?
Seek emergency medical help immediately by calling 911 or your local emergency number. While waiting for help, try to stay calm, rest, and chew aspirin if advised, but avoid self-medicating or driving yourself.
3. Are heart attack symptoms different for men and women?
Yes, symptoms can vary. While men often experience classic symptoms like chest pain and arm discomfort, women may have less typical signs such as nausea, shortness of breath, fatigue, and discomfort in the back or jaw.
4. Can heart attacks happen without any warning?
Yes, heart attacks can occur suddenly without any prior warning signs. However, many people experience subtle symptoms or warning signs in the days or weeks leading up to a heart attack.
5. How can I reduce my risk of a heart attack?
To reduce the risk, adopt a heart-healthy lifestyle: eat a balanced diet, exercise regularly, maintain a healthy weight, manage stress, avoid smoking, and control conditions like high blood pressure and diabetes.
6. Can we give water during a heart attack?
Drinking water during a heart attack is generally not recommended, as it may interfere with urgent medical treatment. Focus on seeking immediate medical help instead of drinking water or attempting self-care measures.
7. What is the first aid of a heart attack?
First aid for a heart attack includes calling emergency services immediately, having the person sit or lie down in a comfortable position, and administering aspirin if recommended by a healthcare provider. Avoid giving them food or drink.
Medical advancements are continually reshaping patient care, with new technologies leading the way to better outcomes. One such innovation is the leadless pacemaker, a miniature device designed to regulate heartbeats without the traditional leads. This technology marks a significant milestone in cardiology, offering numerous benefits over conventional pacemakers. In this blog, we will explore what leadless pacemakers are, how they work, their advantages, and their impact on the future of cardiac care. For those considering this advanced treatment, it is crucial to seek services from the best pacemaker implantation hospital in Noida.
Consult with our experts at the best pacemaker implantation hospital in Noida to explore whether a leadless pacemaker is right for you. Call - +91 9667064100.
A leadless pacemaker is a self-contained device implanted directly into the heart, eliminating the need for leads used in traditional pacemakers. Leads are thin wires that connect the pacemaker to the heart, transmitting electrical impulses to regulate the heartbeat. While effective, these leads can lead to complications such as infections, lead displacement, and breakage. The leadless pacemaker avoids these issues by being directly placed in the heart's right ventricle, where it delivers electrical impulses to maintain a regular heart rhythm.
The leadless pacemaker is implanted through a minimally invasive procedure. A catheter is inserted into a vein in the leg and guided to the heart, where the device is deployed and anchored into the heart tissue. Once in place, the pacemaker continuously monitors the heart's electrical activity and delivers impulses as needed to maintain a regular rhythm.
These devices are powered by a tiny battery designed to last for many years, often comparable to or even longer than traditional pacemakers. The absence of leads significantly reduces the risk of complications, making the procedure safer and the device more reliable.
1. Reduced Complications
One of the primary advantages of the leadless pacemaker is the significant reduction in complications associated with traditional pacemakers. Leads can be a source of various problems, including infection, lead fracture, and displacement. By eliminating leads, the risk of these issues is minimized, leading to improved patient outcomes and reduced need for additional surgeries.
2. Minimally Invasive Procedure
The implantation of a leadless pacemaker is a minimally invasive procedure, typically performed under local anesthesia. This approach results in shorter hospital stays, quicker recovery times, and less discomfort for patients. The procedure is generally less complex and can often be completed in a shorter time compared to traditional pacemaker implantation.
3. Improved Aesthetics and Comfort
Traditional pacemakers require a pocket to be created under the skin to house the device, often leaving a visible bulge and potential for discomfort. The leadless pacemaker, being much smaller and self-contained, does not require such a pocket. This results in a more aesthetically pleasing outcome and greater comfort for the patient, as there is no bulky device under the skin.
4. Longevity and Reliability
Leadless pacemakers are designed to be highly durable and reliable. The elimination of leads reduces the potential points of failure, and the device's battery life is comparable to or exceeds that of traditional pacemakers. This means patients can enjoy the benefits of a reliable heart rhythm management device for many years without the need for frequent replacements.
The introduction of leadless pacemakers represents a significant advancement in cardiac care, offering numerous benefits to patients and healthcare providers alike. Their reduced complication rates, minimally invasive implantation procedure, and improved patient comfort make them a game changer in the field of cardiology.
1. Enhanced Patient Quality of Life
Patients with leadless pacemakers experience fewer complications and quicker recovery times, leading to an overall improvement in their quality of life. The absence of a visible pacemaker pocket and leads also contributes to better aesthetics and comfort, allowing patients to lead more active and fulfilling lives.
2. Cost-Effectiveness
While the initial cost of a leadless pacemaker may be higher than that of a traditional pacemaker, the reduced need for follow-up surgeries and hospitalizations due to complications can make them more cost-effective in the long run. This can lead to significant savings for both patients and healthcare systems.
3. Broader Accessibility
As the technology continues to evolve and become more widely adopted, leadless pacemakers are expected to become more accessible to a larger patient population. This can be particularly beneficial in regions with limited access to advanced cardiac care, as the simplified implantation procedure can be performed in a wider range of healthcare settings.
The development of leadless pacemakers is a testament to the rapid advancements in medical technology. Ongoing research and development efforts are focused on further improving these devices, including extending battery life, enhancing functionality, and expanding their use to a broader range of cardiac conditions.
Future iterations of leadless pacemakers may incorporate additional features such as remote monitoring capabilities, allowing healthcare providers to track device performance and patient health in real-time. This could lead to even more proactive and personalized care, further improving patient outcomes.
Dr. Siddharth Samrat: A distinguished cardiac specialist renowned for his expertise in stent surgeries, Dr. Samrat has successfully performed over 500 coronary angiographies, more than 250 angioplasties, and over 150 pacemaker implantations within just two years. His extensive experience underscores his exceptional skill in advanced cardiac procedures.
Dr. Rahul Arora: With a career spanning over 13 years, Dr. Arora is a highly respected Interventional Cardiologist known for his dedication to patient care and significant contributions to the field of cardiology. His expertise and commitment to advancing cardiac treatment practices have made him a leading figure in the specialty.
Dr. Syed Zafrul Hasan: Bringing more than a decade of experience, Dr. Hasan is a skilled cardiologist proficient in both Non-Invasive (including ECHO, Stress Echo, and TMT) and Invasive Cardiology procedures (such as TPI, Central Line, Arterial Line insertion, and intubation). His extensive knowledge and dedication to comprehensive cardiac care highlight his exceptional capabilities in the field.
Our team at the best pacemaker implantation hospital in Noida is here to provide you with cutting-edge solutions and personalized care. Call - +91 9667064100.
The leadless pacemaker is a revolutionary innovation in the field of Cardiology, offering numerous advantages over traditional pacemakers. Its reduced complication rates, minimally invasive implantation procedure, improved aesthetics, and long-term reliability make it a game changer in cardiac care. As this technology continues to advance and become more widely adopted, it holds the promise of transforming the lives of countless patients, providing them with safer, more effective, and more comfortable heart rhythm management solutions.
If you are considering a pacemaker or have concerns about your heart health, consult with the best cardiologist in Noida to discuss whether a leadless pacemaker may be the right option for you. With ongoing advancements and increasing accessibility, the future of cardiac care looks brighter than ever.
1. What is a leadless pacemaker?
A leadless Pacemaker is a compact, self-contained device implanted directly into the heart without the need for external leads or wires. It is designed to regulate heartbeats by delivering electrical impulses directly to the heart's chambers, typically the right ventricle, to maintain a steady rhythm.
2. What is the difference between a pacemaker and a leadless pacemaker?
Traditional pacemakers consist of a pulse generator connected to the heart by leads or wires that deliver electrical impulses to regulate the heartbeat. In contrast, a leadless pacemaker is a small, battery-powered device implanted directly into the heart. It eliminates the need for external leads, reducing the risk of complications such as infection, lead displacement, or fracture.
3. What is the benefit of a leadless pacemaker?
The primary benefits of a leadless pacemaker include:
4. Who are candidates for a leadless pacemaker?
Candidates for a leadless pacemaker include individuals who:
5. What are the 4 types of pacemakers?
The four main types of pacemakers are:
6. What is the cost of a leadless pacemaker in India?
The cost of a leadless pacemaker in India varies depending on the hospital and the specific model of the device. Generally, the price ranges from ₹2.5 lakh to ₹4 lakh, which includes the device cost and the implantation procedure. Additional expenses for hospital stay and consultations may also apply.
7. What to avoid with a leadless pacemaker?
Patients with a leadless pacemaker should:
8. Which pacemaker is best for the heart?
The best type of pacemaker depends on individual patient needs and specific cardiac conditions. Generally, leadless pacemakers are beneficial for those who need a more minimally invasive option and have no additional requirements that necessitate traditional or biventricular pacemakers. A cardiologist will determine the most suitable pacemaker based on a comprehensive evaluation of the patient’s heart condition, lifestyle, and overall health.
In the realm of cardiovascular medicine, rotablation coronary angiography stands out as an advanced technique for diagnosing and treating complex coronary artery disease. This blog will explore the intricacies of this procedure, its benefits, and what patients in Noida should know about accessing this specialized care.
Care for your heart! Call +91 9667064100 or click here to schedule your consultation with an expert cardiologist.
Before exploring rotablation, let's first understand what coronary angiography is. Coronary angiography is a diagnostic procedure that allows doctors to visualize the blood vessels that supply the heart muscle. During this procedure, a special dye is injected into the coronary arteries, and X-ray images are taken to identify any blockages or narrowing in these vital blood vessels.
Rotablation, also known as rotational atherectomy, is an advanced technique used in conjunction with coronary angiography to treat severely calcified or hardened plaque in the coronary arteries. This procedure uses a tiny, diamond-tipped burr that rotates at high speed to gently sand away hardened plaque, restoring blood flow to the heart.
Precision: The rotablator targets and removes plaque with high accuracy using a high-speed rotating burr. This allows for specific and effective treatment of obstructed areas within the arteries.
Minimally Invasive: Rotablation is performed through a small incision, typically in the wrist or groin, similar to standard angiography. This results in less pain, quicker recovery, and fewer complications compared to open-heart surgery.
Effective for Complex Cases: It is especially useful for treating heavily calcified arteries that are difficult to address with standard balloon angioplasty. Its technique allows for the effective removal of stubborn plaque buildup.
There are many best cardiologists in Noida who are well-versed in determining when rotablation coronary angiography is appropriate. They can evaluate your condition and decide if rotablation is the best treatment for your specific needs. A cardiologist might suggest rotablation coronary angiography in the following situations:
Creatinine levels play a crucial role in determining a patient's eligibility for coronary angiography, including rotablation procedures. Creatinine is a waste product produced by muscle metabolism and is typically filtered out of the blood by the kidneys. In the context of coronary Angiography, kidney function is particularly significant because the contrast dye used during the procedure is eliminated from the body through the kidneys. If the kidneys are not functioning optimally, as indicated by elevated creatinine levels, they may struggle to process and eliminate the contrast dye efficiently.
The decision to proceed with rotablation coronary angiography in patients with high creatinine levels is complex and highly individualized. While elevated creatinine does increase the risk of complications, it doesn't automatically disqualify a patient from the procedure. The decision depends on a careful balance of risks and benefits. In cases where the need for coronary intervention is urgent or critical, such as in acute coronary syndromes, the potential cardiac benefits may outweigh the risks to kidney function. Additionally, the use of rotablation itself doesn't significantly increase the risk compared to standard angiography, as the primary concern is the contrast dye used in both procedures.
In some cases, patients with high creatinine may still undergo the procedure if appropriate precautions are taken and if the potential benefits of the intervention are deemed to outweigh the risks to kidney function.
If your creatinine levels are elevated but coronary angiography is essential, your doctor may take several precautions to protect your kidney function, including:
It's crucial to discuss your kidney function and any concerns about creatinine levels with your cardiologist when considering coronary angiography. They can provide personalized advice based on your overall health status and the necessity of the procedure.
1. Preparation: Prior to the procedure, you will receive a local anesthetic to numb the area and may also be given a mild sedative to help you relax.
2. Access: A small incision is made, typically in your wrist or groin, through which a catheter will be inserted to reach your arteries.
3. Imaging: Contrast dye is introduced into your bloodstream, and X-ray images are captured to visualize and identify any blockages in your arteries.
4. Rotablation: If needed, a rotablator is carefully guided to the blocked area to remove hardened plaque from the artery walls.
5. Additional Treatment: Following rotablation, balloon angioplasty and stenting are often performed to ensure the artery remains open and blood flow is restored.
6. Recovery: After the procedure, you will need to lie flat for several hours to allow the incision site to heal properly and reduce the risk of complications.
Once the recovery period is complete, you may be monitored for a short time to ensure there are no immediate issues. Your doctor will provide you with specific aftercare instructions and schedule follow-up appointments to track your progress and ensure the success of the procedure.
Benefits:
It is essential to have a thorough discussion with your cardiologist to weigh these benefits and risks and to determine whether this procedure is appropriate for your specific condition.
The cost of coronary angiography, particularly when combined with rotablation, can vary widely in Noida. Several factors influence the overall expense:
While it's difficult to provide exact figures due to these variables, Coronary Angiography Cost in Noida typically ranges from ₹25,000 to ₹1,50,000 or more, depending on the factors mentioned above.
Remember, while cost is an important factor, it shouldn't be the only consideration when choosing where to have your procedure done. The expertise of the medical team and the quality of care should be primary considerations.
Dr. Rahul Arora, MBBS, MD, DM, is a distinguished Interventional Cardiologist with over 13 years of extensive experience in cardiology. Known for his dedication and innovation, Dr. Arora excels in rotablation coronary angiography, offering exceptional patient care. His strong academic background and commitment to advancing cardiology make him a standout expert in the field, dedicated to enhancing patient outcomes and advancing the practice of interventional cardiology.
Dr. Syed Zafrul Hasan, MBBS, PGDCC, ACMDC, BLS, ACLS, is a seasoned Interventional Cardiologist with over 13 years of experience. His expertise encompasses both non-invasive procedures, such as ECHO, DSE Stress Echo, and TMT, as well as invasive techniques, including TPI, central line insertion, arterial line insertion, and intubation. Dr. Hasan is well-equipped to address a wide range of cardiac and chronic conditions, including hypertension, diabetes, elevated cholesterol, heart attacks, and peripheral vascular disease.
Dr. Siddharth Samrat, MBBS, MD, DM, is a proficient Cardiologist with two years of experience. He has performed over 500 coronary angiographies, 250+ angioplasties, and 150+ pacemaker implantations. His skills extend to a range of procedures including angioplasty, pacemaker insertion, CRT-D/P, PTMC for mitral stenosis, and device closures. Specializing in complex coronary interventions, coronary imaging, and congenital heart disease, he also treats chronic conditions like hypertension, diabetes, and elevated cholesterol.
Rotablation coronary Angiography represents a significant advancement in the treatment of complex coronary artery disease. For residents of Noida, access to this specialized care is available through several top coronary angiography Hospitals in Noida and skilled cardiologists in the area.
When considering this procedure, it's crucial to research your options thoroughly, considering factors such as hospital reputation, physician experience, and overall cost. By doing so, you can ensure you receive the highest quality care for your heart health needs.
Want to know more about Rotablation? Dial +91 9667064100 or click here for expert guidance!
Is rotablation angioplasty safe?
Rotablation angioplasty is generally considered safe when performed by experienced specialists. It is minimally invasive, but as with any procedure, there are risks involved, including bleeding, infection, and rare complications like heart attack or stroke.
What is the success rate of rotablation?
The success rate of rotablation angioplasty is high, with many patients experiencing significant improvement in blood flow and reduction in symptoms. Success rates can vary based on the complexity of the case and the patient's overall health.
What are the side effects of rotablation?
Side effects of rotablation can include temporary discomfort, bleeding at the catheter insertion site, bruising, and, less commonly, allergic reactions to contrast dye or complications like heart attack or stroke.
Is rotablation painful?
Rotablation is typically performed under local anesthesia and sedation, so patients usually experience minimal pain during the procedure. Some discomfort or soreness at the catheter insertion site may occur afterward, but it is generally manageable.
Which type of angioplasty is best?
The best type of angioplasty depends on the patient's specific condition and the nature of the arterial blockages. Rotablation is ideal for heavily calcified arteries, while balloon angioplasty and stenting may be preferred for other cases.

साइलेंट हार्ट अटैक (Silent Heart Attack) या "साइलेंट मायोकार्डियल इंफार्क्शन" एक ऐसा स्थिति है जिसमें व्यक्ति को दिल के दौरे के सामान्य लक्षण महसूस नहीं होते हैं या वे इतने हल्के होते हैं कि अक्सर नजरअंदाज कर दिए जाते हैं। जानिए इसके लक्षण से लेकर इलाज तक के बारे में विस्तार से..
ज्यादा जानकारी के लिए हमें कॉल करें +91 9667064100.
Table of Contents
साइलेंट हार्ट अटैक (Silent Heart Attack in Hindi), जिसे मूक हृदयाघात (Silent Heart Attack) भी कहा जाता है, एक प्रकार का हृदयाघात होता है जिसमें सामान्य लक्षण जैसे कि छाती में दर्द, सांस की तकलीफ, पसीना आदि महसूस नहीं होते हैं। इसके कारण व्यक्ति को पता नहीं चलता कि उसे हार्ट अटैक हो रहा है। यह स्थिति खासकर उन लोगों के लिए खतरनाक होती है जिन्हें मधुमेह, उच्च रक्तचाप या हृदय रोगों का इतिहास हो।
साइलेंट हार्ट अटैक के लक्षण (Symptoms of Heart Attack in Hindi) बहुत ही सामान्य होते है इनको सही समय से जानना बेहद महत्वपूर्ण है आप भी सही समय से लक्षणों को पहचाने और अपना व अपने परिवार का ध्यान रखें।
स्वस्थ आहार लें:
नियमित व्यायाम करें:
स्वस्थ वजन बनाए रखें:
धूम्रपान और तंबाकू का सेवन बंद करें:
नियमित स्वास्थ्य जांच करवाएं:
तनाव को कम करें:
दवाइयों का सेवन:
पारिवारिक इतिहास पर ध्यान दें:
दवाइयां:
एंजियोप्लास्टी और स्टेंटिंग:
जीवनशैली में बदलाव:
नियमित स्वास्थ्य जांच:
डॉक्टर की सलाह के लिए आज ही फ़ोन करें - +91 9667064100.
साइलेंट हार्ट अटैक के लक्षण पारंपरिक दिल के दौरे की तुलना में कम स्पष्ट होते हैं, जैसे कि हल्का दर्द या असहजता जो सामान्य रूप से ध्यान नहीं जाती। इसका मतलब है कि व्यक्ति को अपनी स्थिति के बारे में जानकारी नहीं होती, जिससे स्थिति और गंभीर हो सकती है। हार्ट अटैक का समय पर इलाज न होना संभावित रूप से गंभीर दिल की बीमारियों की ओर ले जा सकता है। हार्ट अटैक इलाज होना कई जगह बेहद मेहेंगा पद जाता है लेकिन नोएडा में इस इलाज की कीमत हिंदी में (Treatment Cost of Heart Attack in Hindi) जानने के लिए यहाँ पढ़ें।
प्रश्न 1: साइलेंट हार्ट अटैक क्या है ?
उत्तर: साइलेंट हार्ट अटैक एक ऐसी स्थिति है जिसमें दिल के दौरे के लक्षण सामान्य हार्ट अटैक की तरह तीव्र नहीं होते, और व्यक्ति को यह समझ में नहीं आता कि उन्हें हार्ट अटैक हुआ है।
प्रश्न 2: साइलेंट हार्ट अटैक के लक्षण क्या हैं ?
उत्तर: हल्का सीने में दर्द या बेचैनी, थकान या कमजोरी, सांस की तकलीफ, हल्का पसीना आना, पेट दर्द या अपच, गर्दन, जबड़े, या पीठ में हल्का दर्द इलेंट साइलेंट हार्ट अटैक के लक्षण है।
प्रश्न 3: साइलेंट हार्ट अटैक के कारण क्या हैं ?
उत्तर: कोरोनरी धमनियों में रुकावट, उच्च रक्तचाप, उच्च कोलेस्ट्रॉल, धूम्रपान, मधुमेह
साइलेंट हार्ट अटैक के कारण हैं।
प्रश्न 4: साइलेंट हार्ट अटैक का पता कैसे चलता है ?
उत्तर: साइलेंट हार्ट अटैक का पता अक्सर नियमित चिकित्सा जांच के दौरान लगाया जाता है। ईसीजी (ECG), इकोकार्डियोग्राम, और रक्त परीक्षण के माध्यम से इसका निदान किया जा सकता है।
प्रश्न 5: साइलेंट हार्ट अटैक के बाद क्या करना चाहिए ?
उत्तर: साइलेंट हार्ट अटैक के बाद, चिकित्सक की सलाह के अनुसार उपचार और जीवनशैली में बदलाव करना आवश्यक होता है। इसमें दवाइयां लेना, संतुलित आहार, नियमित व्यायाम, धूम्रपान और शराब से बचना शामिल हैं।
प्रश्न 6: साइलेंट हार्ट अटैक को कैसे रोका जा सकता है ?
उत्तर: स्वस्थ आहार का सेवन, नियमित व्यायाम, रक्तचाप और कोलेस्ट्रॉल को नियंत्रित रखना, धूम्रपान और शराब से बचना, नियमित स्वास्थ्य जांच करवाकर साइलेंट हार्ट अटैक को रोका जा सकता है।
प्रश्न 7: किसे साइलेंट हार्ट अटैक का अधिक जोखिम होता है?
उत्तर: वृद्ध लोगों, मधुमेह के रोगियों, उच्च रक्तचाप या उच्च कोलेस्ट्रॉल वाले लोगों, और जिनका पारिवारिक इतिहास हृदय रोगों से जुड़ा हो, उन्हें साइलेंट हार्ट अटैक का अधिक जोखिम होता है।