
Subscribe to our

As winter sets in and temperatures drop, many people eagerly anticipate the holidays, snow days, and cozy nights by the fire. However, amidst the beauty of winter, there lurks a significant health risk that often goes unnoticed: the increased likelihood of hypertension, heart attacks, and strokes. The colder months can have a profound impact on our cardiovascular health, making it crucial to understand these risks for effective prevention and management. This is especially important when considering the need for specialized care, so identifying the best hospital for heart health is essential for anyone at risk during this season.
Consult with your healthcare provider at +91 9667064100 for personalized advice and strategies to stay heart-healthy during the winter months.
Cold weather affects the body in several ways that can increase cardiovascular risks. Understanding these mechanisms is vital for anyone concerned about heart health, especially those with pre-existing conditions such as hypertension or heart disease.
When exposed to cold temperatures, the body naturally responds by constricting blood vessels to maintain core body temperature. This vasoconstriction, while essential for preserving heat, can lead to an increase in blood pressure. As the blood vessels narrow, the heart must pump harder to circulate blood through these constricted pathways, leading to heightened strain on the cardiovascular system.
Cold weather can also lead to an increase in blood viscosity, or thickness. When temperatures drop, the body may produce more red blood cells to compensate for the reduced oxygen levels in cold air. Thicker blood is more difficult to pump and increases the risk of blood clots, which can lead to heart attacks and strokes.
During winter months, people often reduce their physical activity levels due to colder weather and shorter days. Physical inactivity is a known risk factor for hypertension, heart disease, and stroke. When people do exercise in winter, they may engage in more intense activity in a shorter period, which can place additional strain on the heart, particularly in those with pre-existing conditions.
The lack of sunlight during winter can lead to seasonal affective disorder (SAD), a type of depression that can affect motivation and energy levels. This can lead to a sedentary lifestyle and poor dietary choices, both of which are risk factors for hypertension and heart disease.
The holiday season, coupled with the challenges of cold weather, can lead to increased stress and anxiety. Stress triggers the release of hormones such as cortisol, which can elevate blood pressure and heart rate, further increasing the risk of cardiovascular events.
Hypertension
Hypertension, or high blood pressure, is often referred to as a silent killer because it typically has no noticeable symptoms. However, it poses a significant risk for heart disease and stroke. Cold weather can exacerbate hypertension through the mechanisms mentioned earlier. For individuals already diagnosed with hypertension, winter can present additional challenges, such as increased medication needs or the need for more frequent monitoring.
The risk of heart attacks rises significantly during the winter months. According to studies, heart attacks are more prevalent in colder temperatures, especially among individuals with pre-existing heart conditions. The added strain on the heart from increased blood pressure, combined with factors like stress and inactivity, creates a perfect storm for cardiac events.
Similar to heart attacks, the incidence of strokes also increases during the winter. The reasons are multi-faceted, including blood vessel constriction, increased blood viscosity, and the impact of cold temperatures on overall cardiovascular health. Ischemic strokes, caused by blood clots, are particularly linked to cold weather as the likelihood of clot formation rises.
While the risks associated with cold weather are concerning, there are several proactive steps individuals can take to protect their heart health during the winter months.
Layering clothing is key to maintaining body warmth. Ensure that you are well-dressed before going outside in cold temperatures. Protecting your extremities by wearing gloves, socks, and warm hats can help regulate your body temperature and reduce the strain on your cardiovascular system.
For those with hypertension, it’s crucial to monitor blood pressure regularly, especially during the winter months. Keeping track of your readings can help identify any significant changes, allowing for timely intervention. If necessary, consult your healthcare provider to adjust medications or treatment plans as needed.
While it can be tempting to stay indoors during winter, it's important to maintain physical activity. Consider indoor activities such as yoga, home workouts, or even taking brisk walks around your neighborhood when the weather permits. Staying active helps regulate blood pressure and maintain heart health.
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins is essential for heart health. During the winter, comfort foods may be more tempting, but it’s important to prioritize nutrient-dense options that can help manage blood pressure and overall cardiovascular health. Reducing sodium intake and avoiding excessive alcohol consumption can also be beneficial.
Implement stress-reducing techniques such as meditation, deep breathing exercises, or engaging in hobbies that bring joy. It’s essential to find healthy ways to cope with the stress that often accompanies winter and the holiday season. Regular exercise is also an excellent way to manage stress levels.
Cold weather can be deceptive, leading many to forget about hydration. However, staying well-hydrated is essential for overall health, including heart health. Drink plenty of fluids, and remember that caffeine and alcohol can contribute to dehydration, so consume these in moderation.
If you have a history of heart disease, hypertension, or stroke, it’s crucial to consult with a healthcare provider before the winter season. They can offer personalized advice and adjustments to your treatment plan to help mitigate risks during colder months.
As winter approaches, prioritizing your heart health becomes increasingly important. If you have any concerns, consulting with a knowledgeable cardiologist is crucial. At Felix Hospital, our highly skilled team of cardiologists is committed to delivering exceptional care and tailored treatment plans. Among them, Dr. Rahul Arora and Dr. Siddharth Samrat stand out as some of the best cardiologists in Noida, specializing in the diagnosis and management of a wide range of heart conditions. Don’t hesitate to contact us for expert guidance on how to keep your heart healthy during the chilly months ahead.
If you or a loved one is at risk of heart disease, don’t wait for the warning signs—take charge of your heart health today by Clicking Here.
As winter approaches, it's vital to be aware of the potential risks that cold weather poses to your heart health. By understanding how hypertension, heart attacks, and strokes can be exacerbated during this time, you can take proactive steps to protect yourself. From dressing warmly and staying active to maintaining a healthy diet and managing stress, there are numerous ways to reduce your risk. Don't hesitate to seek medical advice if you're concerned about your cardiovascular health, especially if you have pre-existing conditions.
Why does cold weather affect blood pressure?
Cold weather causes blood vessels to constrict, increasing blood pressure as the heart has to work harder to pump blood.
Are heart attacks more common in winter?
Yes, studies show that heart attacks are more prevalent during colder months due to factors such as increased blood pressure and inactivity.
What can I do to stay active in the winter?
Indoor activities like yoga, gym workouts, or even brisk walking when weather permits can help maintain physical activity levels.
How can I manage stress during the winter?
Techniques such as meditation, deep breathing, and engaging in enjoyable hobbies can help reduce stress levels.
Should I adjust my diet in winter?
Yes, focusing on a balanced diet rich in nutrients while limiting sodium and processed foods can help maintain heart health during colder months.
How often should I monitor my blood pressure in winter?
Regular monitoring is recommended, especially if you have hypertension. Check with your healthcare provider for personalized advice.
Is dehydration a concern in winter?
Yes, cold weather can lead to dehydration. It's essential to drink plenty of fluids, even if you don't feel thirsty.
What should I do if I experience chest pain in winter?
Seek immediate medical attention if you experience chest pain, especially if it is accompanied by other symptoms of a heart attack.
Can stress lead to heart problems?
Yes, chronic stress can contribute to high blood pressure and increase the risk of heart disease and stroke. Finding healthy coping strategies is essential.

सर्दियों के मौसम में दिल के दौरे का खतरा अधिक बढ़ जाता है और इसके पीछे कई कारण होते हैं। ठंड का असर खासतौर पर दिल और रक्तवाहिकाओं पर पड़ता है। इन कारणों से सर्दियों में विशेष सावधानी बरतने की आवश्यकता होती है, खासकर दिल की बीमारियों से पीड़ित लोगों के लिए। हार्ट अटैक के सामान्य लक्षणों में सीने में दर्द या भारीपन, सांस लेने में कठिनाई, ठंडे पसीने आना, चक्कर आना और कंधे, गर्दन या बाजू में दर्द शामिल होते हैं। अगर ये लक्षण दिखें, तो तुरंत सबसे अच्छा हार्ट अटैक अस्पताल से चिकित्सकीय सहायता लें।
ज्यादा जानकारी के लिए हमें कॉल करें +91 9667064100.
सर्दियों के मौसम में हार्ट अटैक का खतरा क्यों बढ़ता है ? (Why does the risk of heart attack increase in winter season)
सर्दियों के मौसम में हार्ट अटैक के लक्षण (Symptoms of heart attack in winter season)
सर्दियों के मौसम में हार्ट अटैक के कारण (Causes of heart attack in winter season)
सर्दियों के मौसम में हार्ट अटैक से बचाव (Heart attack prevention in winter season)
सर्दियों के मौसम में हार्ट अटैक का इलाज (Treatment of heart attack in winter season)
फेलिक्स हॉस्पिटल्स में हार्ट अटैक के विशेषज्ञ के बारे में जानें (Know the heart attack expert at felix hospitals)
निष्कर्ष (Conclusion)
सर्दियों के मौसम में हार्ट अटैक को लेकर अक्सर पूछे जाने वाले सवाल और जवाब ( Frequently asked questions and answers regarding heart attack in winter season)
रक्त वाहिकाओं का सिकुड़ना:
ठंड के मौसम में शरीर की रक्त वाहिकाएं सिकुड़ जाती हैं, जिससे रक्त का प्रवाह धीमा हो जाता है और रक्तचाप बढ़ जाता है। इससे दिल को अधिक मेहनत करनी पड़ती है, जो हार्ट अटैक का कारण बन सकता है।
रक्त का गाढ़ा होना:
सर्दियों में शरीर का तापमान गिरने पर खून गाढ़ा हो सकता है, जिससे थक्के बनने का खतरा बढ़ जाता है। अगर यह थक्का हृदय की धमनियों में फंस जाता है, तो दिल के दौरे हो सकता है।
बढ़ा हुआ रक्तचाप:
ठंड में ब्लड प्रेशर स्वाभाविक रूप से बढ़ जाता है क्योंकि दिल को शरीर को गर्म रखने के लिए अधिक प्रयास करना पड़ता है। यह भी हार्ट अटैक के जोखिम को बढ़ाता है।
कम शारीरिक गतिविधि:
सर्दियों में लोग आमतौर पर कम चलते-फिरते हैं, जिससे उनका शारीरिक स्वास्थ्य बिगड़ सकता है। यह दिल के लिए जोखिम भरा हो सकता है क्योंकि शारीरिक गतिविधि की कमी से कोलेस्ट्रॉल का स्तर बढ़ सकता है।
ठंड के कारण ऑक्सीजन की कमी:
ठंडे मौसम में शरीर को अतिरिक्त ऊर्जा की आवश्यकता होती है, जिससे ऑक्सीजन की मांग बढ़ जाती है। अगर शरीर को पर्याप्त ऑक्सीजन नहीं मिलती, तो दिल को अतिरिक्त दबाव सहना पड़ता है, जिससे दिल के दौरे का खतरा बढ़ जाता है।
सर्दियों में तनाव:
सर्दी के मौसम में तनाव और अवसाद भी बढ़ जाते हैं, जो हार्ट अटैक के जोखिम को बढ़ा सकते हैं। तनाव से रक्तचाप और हार्मोनल असंतुलन बढ़ सकता है, जो दिल पर बुरा असर डालता है।
सीने में दर्द या असहजता:
सीने के बीच या बाईं ओर भारीपन, दबाव या जलन जैसा महसूस होना। दर्द अक्सर कुछ मिनटों तक रहता है और फिर कम या अधिक हो सकता है। यह दिल के दौरे का प्रमुख लक्षण होता है।
बांह, गर्दन, या जबड़े में दर्द:
दर्द या असहजता सीने से कंधे, बाईं बांह, पीठ, गर्दन या जबड़े तक फैल सकती है। यह दर्द कभी-कभी बाईं ओर अधिक महसूस होता है।
सांस लेने में कठिनाई:
सामान्य से अधिक गहरी या कठिनाई से सांस लेना हार्ट अटैक का संकेत हो सकता है, खासकर जब इसे बिना किसी स्पष्ट कारण के अनुभव किया जाए।
ठंडे पसीने आना:
अचानक ठंडे पसीने का आना दिल के दौरे के चेतावनी संकेतों में से एक है, खासकर सर्दी के मौसम में जब शरीर पहले से ठंडे वातावरण में हो।
थकान या कमजोरी:
बिना किसी भारी शारीरिक गतिविधि के अत्यधिक थकान महसूस होना या कमजोरी महसूस होना यह खासकर महिलाओं में हार्ट अटैक का सामान्य लक्षण हो सकता है।
चक्कर आना या बेहोशी:
चक्कर आना, हल्का महसूस होना या बेहोश होने जैसा महसूस होना दिल के दौरे का एक संकेत हो सकता है, जो सर्दी में कम ऑक्सीजन के कारण और अधिक गंभीर हो सकता है।
जी मिचलाना या उल्टी आना:
हार्ट अटैक के दौरान कुछ लोगों को मिचली या उल्टी का अनुभव भी हो सकता है। यह लक्षण अक्सर अन्य पाचन समस्याओं की तरह लग सकता है लेकिन दिल की समस्या का संकेत हो सकता है।
पेट में दर्द या असहजता:
कुछ लोगों में दिल के दौरे के दौरान पेट में दर्द या जलन हो सकती है। इसे एसिडिटी या अपच समझने की गलती भी की जा सकती है।
रक्त वाहिकाओं का सिकुड़ना:
ठंड के मौसम में शरीर की रक्त वाहिकाएं सिकुड़ जाती हैं, जिससे रक्तचाप बढ़ जाता है। इससे दिल को शरीर में रक्त पंप करने के लिए अधिक मेहनत करनी पड़ती है, जो दिल पर अतिरिक्त दबाव डालता है और हार्ट अटैक का खतरा बढ़ जाता है।
रक्त का गाढ़ा होना:
सर्दियों में ठंड के कारण खून गाढ़ा हो जाता है, जिससे थक्के बनने का खतरा बढ़ जाता है। यह थक्के रक्त वाहिकाओं में अवरोध पैदा कर सकते हैं, जिससे दिल को रक्त प्रवाह बाधित हो जाता है और हार्ट अटैक हो सकता है।
ब्लड प्रेशर का बढ़ना:
ठंडे मौसम में शरीर को गर्म रखने के लिए रक्तचाप स्वाभाविक रूप से बढ़ जाता है। उच्च रक्तचाप हार्ट अटैक का प्रमुख जोखिम कारक होता है, क्योंकि इससे हृदय की धमनियों पर अधिक दबाव पड़ता है।
शारीरिक गतिविधियों में कमी:
सर्दियों में लोग सामान्यत कम शारीरिक गतिविधियां करते हैं, जिससे वजन बढ़ सकता है और मेटाबॉलिज्म धीमा हो जाता है। शारीरिक गतिविधियों की कमी से दिल की सेहत खराब होती है और हार्ट अटैक का खतरा बढ़ सकता है।
ऑक्सीजन की कमी:
ठंडे मौसम में शरीर की ऑक्सीजन की जरूरत बढ़ जाती है, लेकिन ठंड के कारण खून में ऑक्सीजन का स्तर कम हो सकता है। दिल को अधिक ऑक्सीजन की आवश्यकता होती है, और इसकी कमी से दिल पर अतिरिक्त दबाव पड़ता है, जिससे दिल के दौरे का खतरा बढ़ जाता है।
मानसिक तनाव और अवसाद:
सर्दियों में दिन छोटे होते हैं और सूरज की रोशनी कम मिलती है, जिससे कुछ लोगों में मानसिक तनाव और अवसाद (सीजनल अफेक्टिव डिसऑर्डर) बढ़ सकता है। तनाव और अवसाद हार्ट अटैक के जोखिम को बढ़ाने वाले कारकों में से एक होते हैं, क्योंकि ये ब्लड प्रेशर और दिल की धड़कन को प्रभावित करते हैं।
धूम्रपान और शराब का बढ़ा हुआ सेवन:
सर्दियों में कुछ लोग धूम्रपान और शराब का सेवन बढ़ा देते हैं ताकि उन्हें ठंड से राहत मिले। धूम्रपान और अत्यधिक शराब दिल के लिए हानिकारक होते हैं और इससे हार्ट अटैक का खतरा बढ़ जाता है।
अचानक तापमान परिवर्तन:
सर्दियों में ठंडे वातावरण से अचानक गर्म वातावरण में जाना या ठंडे पानी से नहाना दिल पर अचानक दबाव डाल सकता है। यह तापमान में अचानक बदलाव दिल को झटका दे सकता है और दिल के दौरे का कारण बन सकता है।
अधिक कैलोरी युक्त भोजन:
सर्दियों में लोग अधिक कैलोरी और वसायुक्त भोजन करना पसंद करते हैं, जिससे कोलेस्ट्रॉल का स्तर बढ़ सकता है। उच्च कोलेस्ट्रॉल से धमनियां संकरी हो जाती हैं, जो दिल के दौरे का खतरा बढ़ाता है।
तुरंत चिकित्सा सहायता प्राप्त करें:
अगर दिल के दौरे के लक्षण दिखाई दें (जैसे कि सीने में दर्द, सांस की कमी, ठंडे पसीने आना), तो तुरंत आपातकालीन चिकित्सा सेवा को बुलाएं। हार्ट अटैक का समय पर इलाज बहुत महत्वपूर्ण होता है, क्योंकि पहले 1 घंटे में इलाज मिलने से गंभीर नुकसान को रोका जा सकता है।
प्राथमिक उपचार :
हार्ट अटैक के दौरान एस्पिरिन की एक गोली (300mg) चबाकर खाई जा सकती है लेकिन अगर डॉक्टर ने इसे अनुमति दी हो तो। क्योंकि एस्पिरिन खून को पतला करने में मदद करती है और थक्के बनने से रोकती है। अगर मरीज के पास नाइट्रोग्लिसरीन है जो दिल की बीमारी के मरीजों को डॉक्टर द्वारा दी जाती है, तो इसे निर्देशानुसार लिया जा सकता है ताकि दिल की धमनियों को आराम मिल सके। इन प्राथमिक उपचारों के बाद जल्द से जल्द अस्पताल पहुंचने की कोशिश करें।
चिकित्सीय उपचार (Medical Treatment) :
खून में बने थक्के को घोलने के लिए थ्रोम्बोलिटिक दवाओं का इस्तेमाल किया जाता है, जो ब्लड फ्लो को पुनः सामान्य बनाने में मदद करती है। इसे क्लॉट-बस्टर दवा भी कहा जाता है।
एंजियोप्लास्टी और स्टेंटिंग:
अगर दिल के दौरे का कारण किसी धमनियों में रुकावट है, तो डॉक्टर एंजियोप्लास्टी कर सकते हैं। इस प्रक्रिया में धमनियों को चौड़ा करने के लिए एक छोटी सी ट्यूब (स्टेंट) डाली जाती है ताकि ब्लड फ्लो ठीक हो सके।
कोरोनरी आर्टरी बाईपास ग्राफ्ट (CABG):
यह सर्जरी उन मामलों में की जाती है जब धमनियों में रुकावट को हटाना मुश्किल होता है। इसमें डॉक्टर खून के प्रवाह को सुनिश्चित करने के लिए हृदय की बंद धमनियों को बाईपास कर देते हैं।
मेडिकल मैनेजमेंट:
एंटीप्लेटलेट दवाएं जैसे एस्पिरिन, क्लोपिडोग्रेल दी जाती हैं ताकि खून में थक्के बनने से रोका जा सके। बीटा-ब्लॉकर्स दिल की धड़कन को धीमा कर हृदय की ऑक्सीजन की जरूरत को कम करती हैं। कोलेस्ट्रॉल-घटाने वाली दवाएं जैसे स्टेटिन्स हृदय की धमनियों में कोलेस्ट्रॉल जमने को रोकती हैं।
पुनर्वास (Rehabilitation)
डॉक्टर की देखरेख में व्यायाम और पोषण से जुड़े कार्यक्रम, जिनका उद्देश्य हृदय की सेहत में सुधार करना और हार्ट अटैक की पुनरावृत्ति को रोकना होता है। दिल को स्वस्थ रखने के लिए संतुलित आहार, नियमित व्यायाम, तनाव प्रबंधन, धूम्रपान और शराब से परहेज करना चाहिए।
ठंड से बचाव:
मरीज को सर्दी में अतिरिक्त गर्म कपड़ों से ढक कर रखना चाहिए ताकि ठंड के प्रभाव से रक्त वाहिकाएं संकुचित न हों।
ठंडी हवा से बचें:
दिल के दौरे के दौरान ठंडी हवा दिल पर अतिरिक्त दबाव डाल सकती है, इसलिए मरीज को गर्म वातावरण में रखना चाहिए।
व्यायाम करते समय सावधानी:
हार्ट अटैक के बाद पुनर्वास के दौरान सर्दियों में बाहर व्यायाम करते समय सावधानी बरतनी चाहिए। ठंड में अचानक शारीरिक गतिविधि दिल पर दबाव डाल सकती है।
शारीरिक गतिविधि बनाए रखें:
सर्दियों में शारीरिक रूप से सक्रिय रहना बहुत महत्वपूर्ण है। नियमित व्यायाम करने से रक्त संचार में सुधार होता है और दिल को मजबूत बनाए रखने में मदद मिलती है। हल्की-फुल्की सैर, योग और स्ट्रेचिंग जैसी गतिविधियाँ फायदेमंद हो सकती हैं। हालांकि, अत्यधिक ठंड में बाहर व्यायाम करने से बचें और शरीर को ज्यादा ठंड में न डालें।
पर्याप्त गर्म कपड़े पहनें:
सर्दियों में शरीर को गर्म रखना बेहद जरूरी है। ठंडे मौसम में उचित गर्म कपड़े पहनें, जैसे ऊनी कपड़े, मोजे, और दस्ताने। सिर को टोपी से ढककर रखें, क्योंकि शरीर की अधिकांश गर्मी सिर से निकलती है। तापमान में अचानक गिरावट से बचने के लिए घर से बाहर निकलते समय हमेशा गर्म कपड़े पहनें।
धूम्रपान और शराब से बचें:
धूम्रपान और शराब का सेवन दिल के लिए बहुत हानिकारक हो सकता है, खासकर सर्दियों में। धूम्रपान से रक्त वाहिकाएं सिकुड़ जाती हैं और रक्तचाप बढ़ जाता है, जिससे दिल के दौरे का खतरा बढ़ जाता है। इसी तरह, शराब दिल की धड़कन को असामान्य कर सकती है, जिससे दिल पर अतिरिक्त दबाव पड़ता है।
संतुलित आहार लें:
सर्दियों में वसायुक्त और तैलीय भोजन से बचें, क्योंकि इससे कोलेस्ट्रॉल का स्तर बढ़ सकता है, जो दिल के लिए हानिकारक होता है। अधिक फल, सब्जियां और फाइबर युक्त आहार लें। ओमेगा-3 फैटी एसिड से भरपूर भोजन (जैसे मछली, अलसी के बीज) और अच्छे वसा का सेवन दिल के लिए लाभकारी होता है।
सर्दियों में रक्तचाप और कोलेस्ट्रॉल के स्तर को नियंत्रित रखना बहुत जरूरी है। अगर आप पहले से ही उच्च रक्तचाप या हृदय रोग से पीड़ित हैं, तो नियमित रूप से डॉक्टर से जांच कराएं और अपनी दवाएं समय पर लें। सर्दियों में अपने ब्लड प्रेशर पर नजर रखें।
ठंड से सीधे संपर्क से बचें:
बहुत ठंडे मौसम में बाहर जाने से बचें, खासकर तब जब हवा ठंडी हो। अगर बाहर जाना आवश्यक हो तो नाक और मुंह को स्कार्फ या मास्क से ढक लें, ताकि ठंडी हवा सीधे फेफड़ों में न जाए। ठंड में अचानक से ज्यादा मेहनत वाला काम न करें, क्योंकि इससे दिल पर जोर पड़ सकता है।
तनाव और अवसाद को नियंत्रित करें:
सर्दियों में मानसिक तनाव और अवसाद (सीजनल अफेक्टिव डिसऑर्डर) का सामना करना सामान्य हो सकता है। इसलिए मानसिक स्वास्थ्य का ध्यान रखें। योग, ध्यान, और अन्य रिलैक्सेशन तकनीकों का अभ्यास करें ताकि तनाव से बचा जा सके। परिवार और दोस्तों से बातचीत करना और सामाजिक गतिविधियों में शामिल रहना भी मानसिक स्वास्थ्य के लिए अच्छा होता है।
अधिक पानी पीएं:
सर्दियों में लोग अक्सर कम पानी पीते हैं, जिससे शरीर में डिहाइड्रेशन हो सकता है। शरीर को हाइड्रेटेड रखने से रक्तचाप नियंत्रित रहता है और रक्त का प्रवाह सुचारू रहता है। ठंड में भी पर्याप्त पानी पिएं, चाहे आपको प्यास न लगे।
ठंड में भारी शारीरिक कार्य करने से बचें :
सर्दियों में भारी वजन उठाने या बहुत ज्यादा मेहनत करने से बचें, क्योंकि ठंड में दिल पर दबाव अधिक होता है। अगर आपको कोई शारीरिक कार्य करना हो, तो पहले शरीर को गर्म करके ही काम शुरू करें।
दवाइयों और सलाह का पालन करें:
अगर आप पहले से दिल की बीमारी या उच्च रक्तचाप जैसी समस्याओं से जूझ रहे हैं, तो डॉक्टर द्वारा बताई गई दवाइयों और सलाह का पालन करें। सर्दियों में नियमित रूप से डॉक्टर की सलाह लें और कोई भी असामान्य लक्षण दिखने पर तुरंत चिकित्सा सहायता प्राप्त करें।
हार्ट अटैक के इलाज के लिए विभिन्न विशेषज्ञों की टीम आवश्यक होती है। फेलिक्स हॉस्पिटल्स के कार्डयोलॉजिस्ट्स जो सर्वोत्तम हृदय शल्यचिकित्सक, डॉ. राहुल अरोरा और डॉ. सिद्धार्थ सम्राट से मिलकर आप अपने हार्ट अटैक का इलाज जान सकते हैं। कार्डियोलॉजिस्ट, इंटरवेंशनल कार्डियोलॉजिस्ट, हार्ट सर्जन (कार्डियक सर्जन), इमरजेंसी मेडिसिन डॉक्टर, इंटेंसिविस्ट (आईसीयू डॉक्टर) के अलावा नर्स और पैरामेडिक्स देखभाल और उपचार में सहायता करते हैं।
फेलिक्स हॉस्पिटल में कार्डियोलॉजिस्ट डॉक्टर की सलाह के लिए आज ही फोन करें +91 9667064100.
सर्दियों के मौसम में दिल के दौरे का इलाज अन्य मौसमों में होने वाले हार्ट अटैक के इलाज से बहुत हद तक समान होता है, लेकिन ठंड के मौसम में कुछ अतिरिक्त सावधानियाँ बरतनी पड़ सकती हैं। हार्ट अटैक के दौरान समय पर और सही उपचार दिल के दौरे के गंभीर परिणामों को रोक सकता है। सर्दियों में दिल के दौरे के इलाज के लिए समय पर और उचित चिकित्सा सहायता अत्यधिक आवश्यक है। दिल के दौरे के बाद दी जाने वाली देखभाल और जीवनशैली में सुधार भविष्य में दिल के दौरे को रोकने में मदद कर सकते हैं।
प्रश्न 1: सर्दियों में हार्ट अटैक का खतरा क्यों बढ़ जाता है ?
उत्तर: र्दियों में ठंड के कारण रक्त वाहिकाएं सिकुड़ जाती हैं, जिससे रक्तचाप बढ़ता है और दिल पर अधिक दबाव पड़ता है। इसके अलावा ठंड से खून गाढ़ा हो जाता है, जिससे थक्के बनने का खतरा होता है, और ऑक्सीजन की कमी भी दिल के लिए हानिकारक हो सकती है।
प्रश्न 2: क्या ठंड में ज्यादा व्यायाम करने से दिल पर खतरा बढ़ सकता है ?
उत्तर: सर्दी में अत्यधिक और अचानक व्यायाम करने से दिल पर दबाव बढ़ सकता है। अगर आप पहले से हार्ट की बीमारी से पीड़ित हैं, तो अचानक भारी व्यायाम करने से बचें और किसी भी नए व्यायाम को शुरू करने से पहले डॉक्टर की सलाह लें।
प्रश्न 3: सर्दियों में ब्लड प्रेशर क्यों बढ़ता है ?
उत्तर: ठंडे मौसम में रक्त वाहिकाएं सिकुड़ जाती हैं, जिससे रक्त प्रवाह में बाधा उत्पन्न होती है और ब्लड प्रेशर बढ़ जाता है। उच्च रक्तचाप दिल की बीमारियों और हार्ट अटैक के खतरे को बढ़ा सकता है।
प्रश्न 4: क्या दिल के मरीजों को सर्दियों में बाहर जाने से बचना चाहिए ?
उत्तर: दिल के मरीजों को बहुत ठंडे मौसम में बाहर जाने से बचना चाहिए, खासकर अगर तापमान बहुत कम हो। अगर बाहर जाना आवश्यक हो, तो पूरी तरह से गर्म कपड़े पहनें और शरीर को गर्म रखने के उपाय करें। ठंड के समय अचानक शारीरिक गतिविधियां करने से भी बचें।
प्रश्न 5: क्या ठंडे पानी में नहाने से हार्ट अटैक का खतरा बढ़ सकता है ?
उत्तर: हां, ठंडे पानी में नहाने से शरीर में अचानक तापमान में गिरावट होती है, जिससे दिल पर अचानक दबाव पड़ सकता है और हार्ट अटैक का खतरा बढ़ सकता है। सर्दियों में गुनगुने पानी से नहाना बेहतर होता है, खासकर बुजुर्गों और दिल के मरीजों के लिए।
प्रश्न 6: क्या सर्दियों में डाइट में कुछ बदलाव करना चाहिए ?
उत्तर: हां, सर्दियों में ऐसा आहार लें जो शरीर को गर्म रखे और पोषक तत्वों से भरपूर हो। साबुत अनाज, फल, सब्जियां, ओमेगा-3 फैटी एसिड युक्त खाद्य पदार्थ और हरी पत्तेदार सब्जियाँ दिल के लिए फायदेमंद होती हैं। तैलीय और वसायुक्त भोजन से बचें।
प्रश्न 7: क्या विटामिन डी की कमी भी हार्ट अटैक के खतरे को बढ़ाती है ?
उत्तर: हां, सर्दियों में सूरज की रोशनी कम मिलने से विटामिन डी की कमी हो सकती है, जो दिल की सेहत को प्रभावित कर सकती है। विटामिन डी की कमी से उच्च रक्तचाप और हार्ट अटैक का खतरा बढ़ सकता है। इसलिए, विटामिन डी युक्त खाद्य पदार्थों का सेवन करें या डॉक्टर की सलाह पर सप्लीमेंट लें।
प्रश्न 8: ठंड में मानसिक तनाव और हार्ट अटैक का क्या संबंध है ?
उत्तर: सर्दियों में दिन छोटे और अंधेरे अधिक होने से कुछ लोगों में मानसिक तनाव और अवसाद बढ़ सकता है, जिससे ब्लड प्रेशर बढ़ता है और हार्ट अटैक का खतरा बढ़ सकता है। मानसिक तनाव को कम करने के लिए नियमित व्यायाम, ध्यान और दोस्तों या परिवार के साथ समय बिताना फायदेमंद हो सकता है।

In today's fast-paced corporate world, stress has become an unavoidable part of daily life for many professionals. While some levels of stress can serve as a motivating factor, chronic stress can lead to severe implications for both mental and physical health. Among the various health concerns linked to prolonged stress, cardiovascular diseases—particularly heart disease—are among the most alarming. Understanding how corporate stress impacts heart health is vital for employees and employers alike, as it can help foster a healthier workplace culture. For those seeking guidance and treatment for stress-related heart issues, consulting the best hospital for heart health can provide the necessary support and resources for maintaining overall well-being.
Take Charge of Your Heart Health Today! Consult with healthcare professionals at the best hospital for heart health by Calling +91 9667064100.
Corporate stress is the pressure employees face in their professional environments, often arising from high workloads, tight deadlines, job insecurity, and interpersonal conflicts. This type of stress can trigger the body’s fight-or-flight response, releasing hormones like adrenaline and cortisol, which can be beneficial in short bursts. However, chronic exposure to stress can lead to negative health outcomes.
When you experience stress, your body enters a state of heightened alertness. The heart rate increases, blood vessels constrict, and blood pressure rises, all of which are designed to prepare you for immediate action. However, if stress persists over time, these physiological responses can lead to significant cardiovascular issues:
1. Increased Blood Pressure: Chronic stress can contribute to long-term hypertension, a leading risk factor for heart disease.
2. Inflammation: Stress triggers inflammation in the body, which can damage blood vessels and lead to atherosclerosis (the buildup of plaques in arteries).
3. Unhealthy Coping Mechanisms: Individuals under chronic stress may turn to unhealthy habits, such as smoking, excessive alcohol consumption, or poor dietary choices, which further exacerbate heart problems.
4. Impaired Heart Function: Long-term stress can lead to structural and functional changes in the heart, increasing the risk of heart attacks and heart failure.
The consequences of corporate stress on heart health are substantial. Some of the key risks include:
1. Heart Disease: Prolonged stress can significantly increase the likelihood of developing coronary artery disease, heart attacks, and arrhythmias.
2. Stroke: High stress levels can contribute to conditions that raise the risk of stroke, including hypertension and atherosclerosis.
3. Cardiovascular Events: Stress can trigger acute cardiovascular events, such as heart attacks, especially in individuals with existing heart conditions.
4. Mental Health Disorders: Stress often leads to anxiety and depression, both of which are linked to higher cardiovascular risk.
5. Reduced Quality of Life: The impact of chronic stress extends beyond physical health, affecting overall quality of life, productivity, and workplace morale.
Addressing corporate stress is essential for protecting heart health. Here are some effective treatment strategies:
Engaging with a mental health professional can help individuals develop coping mechanisms to manage stress. Cognitive-behavioral therapy (CBT) is particularly effective in addressing stress-related issues.
Organizations can implement stress management programs that provide employees with tools to cope with stress effectively. These may include workshops, seminars, and training sessions focused on mindfulness, time management, and relaxation techniques.
In some cases, healthcare providers may prescribe medications to manage anxiety or depression linked to stress. Antidepressants and anti-anxiety medications can help stabilize mood and reduce stress levels.
Encouraging a healthy lifestyle can significantly mitigate the effects of corporate stress on heart health. Recommendations include:
Regular Exercise: Engaging in physical activity releases endorphins, which can enhance mood and reduce stress. Aim for at least 150 minutes of moderate aerobic activity each week.
Balanced Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can improve overall well-being and heart health.
Adequate Sleep: Quality sleep is essential for stress management and heart health. Aim for 7-9 hours of uninterrupted sleep each night. Techniques such as meditation, yoga, and deep-breathing exercises can help individuals relax and manage stress effectively.
Mindfulness Practices: Techniques such as meditation, yoga, and deep-breathing exercises can help individuals relax and manage stress effectively.
Employers can play a significant role in mitigating stress by creating a supportive work environment. Implementing wellness programs that promote physical and mental health, such as fitness challenges, mental health days, and flexible work arrangements, can foster a healthier workplace culture.
Preventing corporate stress requires a proactive approach, both individually and organizationally. Here are some effective prevention tips:
Creating an open and transparent communication channel within the workplace allows employees to express their concerns and challenges. This can reduce feelings of isolation and help management address stressors effectively.
Encouraging employees to maintain a healthy work-life balance can reduce stress and improve job satisfaction. Flexible work hours, remote work options, and adequate time off can help employees recharge.
A supportive workplace culture can significantly impact employee well-being. Promoting teamwork, recognizing achievements, and encouraging camaraderie can create a more positive atmosphere.
EAPs provide employees with access to counseling services, financial advice, and stress management resources. These programs can help individuals address personal and professional challenges effectively.
Encouraging employees to have regular health screenings can help identify risk factors associated with stress and heart health. Early detection and intervention are key to preventing serious health issues.
Providing training and development opportunities can help employees feel valued and engaged in their work. This can lead to increased job satisfaction and reduced stress levels.
If you are experiencing stress-related heart health issues, consulting with the best heart specialist is crucial. At Felix Hospital, we prioritize your cardiovascular health and offer a range of services to address your needs. Our team of experienced cardiologists including Dr. Rahul Arora and Dr. Siddharth Samrat specialize in diagnosing and treating heart-related conditions linked to stress. Don't hesitate to reach out to us for personalized care and treatment plans that focus on your well-being.
Scheduling a consultation with a specialist at the best hospital for heart health to learn more by Clicking Here.
In conclusion, corporate stress significantly impacts heart health, increasing the risks of hypertension, heart attacks, and strokes. Understanding the connection between stress and cardiovascular health is essential for both employees and employers. By implementing effective treatment strategies, and preventive measures, and promoting a supportive work environment, we can mitigate the effects of stress and protect heart health. Remember, taking proactive steps to manage stress and prioritize your heart health is not only beneficial for your well-being but also enhances productivity and morale in the workplace.
1. What are the signs of stress affecting heart health?
Ans: Signs may include chest pain, shortness of breath, rapid heartbeat, anxiety, and fatigue.
2. How can I manage work-related stress?
Ans: Techniques include time management, physical activity, mindfulness practices, and seeking support from colleagues or professionals.
3. Are there specific diets that can help with stress management?
Ans: A balanced diet rich in fruits, vegetables, whole grains, and healthy fats can help manage stress and support heart health.
4. When should I consult a doctor about my stress?
Ans: If stress significantly impacts your daily life or leads to physical symptoms, it’s important to seek medical advice.
5. Can corporate wellness programs reduce stress levels?
Ans: Yes, effective wellness programs can create a supportive work environment and provide employees with tools to manage stress.
6. What lifestyle changes can reduce heart disease risk?
Ans: Regular exercise, a heart-healthy diet, adequate sleep, and stress management techniques can lower heart disease risk.
7. How does chronic stress lead to high blood pressure?
Ans: Chronic stress triggers the release of hormones that can constrict blood vessels and raise blood pressure over time.
8. Can relaxation techniques improve heart health?
Ans: Yes, techniques such as meditation, deep-breathing exercises, and yoga can reduce stress levels and improve heart health.
9. What role do employers play in managing employee stress?
Ans: Employers can foster a supportive work environment, promote work-life balance, and provide resources for stress management and health care.

As winter descends and temperatures drop, many people find joy in the season’s festivities. However, for individuals with pre-existing heart conditions or risk factors for heart disease, winter can also pose serious health risks. Research has shown that the risk of heart attacks increases significantly during the colder months. Understanding the reasons behind this trend and adopting preventive measures can help reduce the risk of cardiac arrest. Let’s explore how cold weather affects heart health and provide practical tips to stay safe during the winter months with the help of the best heart attack treatment hospital in Noida.
Contact us today at +91 9667064100 to schedule a consultation and prioritize your heart health!
Cold temperatures can have several effects on the cardiovascular system. When exposed to cold, blood vessels constrict to preserve heat, leading to increased blood pressure. This constriction means the heart must work harder to pump blood, elevating the workload on the heart. For individuals with existing heart conditions, this added strain can be dangerous.
Furthermore, cold weather can lead to changes in behavior that can increase heart attack risk. Many people become less active during the winter months, which can contribute to weight gain and a decline in cardiovascular fitness. Additionally, the holiday season often brings about increased stress, poor dietary choices, and excessive alcohol consumption, all of which can negatively impact heart health.
Certain populations are particularly vulnerable to heart attacks in winter, including:
Individuals with Pre-existing Heart Conditions: Those with a history of heart disease, previous heart attacks, or heart failure are at a greater risk during colder months.
Older Adults: Age is a significant factor, as the heart and blood vessels can become less resilient over time, making older individuals more susceptible to heart-related issues.
Diabetics: People with diabetes often face increased cardiovascular risks, and cold weather can exacerbate these conditions.
Individuals with High Blood Pressure or High Cholesterol: Those who struggle with hypertension or elevated cholesterol levels should be particularly cautious during the winter.
Understanding the symptoms of a heart attack is crucial, especially during the winter months. Common symptoms include:
Chest Pain or Discomfort: This may feel like pressure, squeezing, fullness, or pain in the center or left side of the chest. It can last for more than a few minutes or go away and return.
Shortness of Breath: This may occur with or without chest discomfort and can happen during rest or physical activity.
Radiating Pain: Discomfort may spread to the shoulders, neck, arms, back, teeth, or jaw.
Other Symptoms: These can include lightheadedness, nausea, cold sweats, or unusual fatigue, especially in women.
If you or someone you know experiences these symptoms, seek emergency medical attention immediately.
While it’s impossible to eliminate all risks associated with heart attacks during winter, several strategies can help mitigate them. Here are some practical steps to keep your heart healthy in the cold:
When heading outdoors in winter, dressing in layers is essential. Wear insulated and breathable clothing to keep your body warm without overheating. Pay special attention to your extremities; wearing hats, gloves, and warm socks can help maintain overall body temperature and prevent heat loss.
Physical activity is crucial for heart health. During the winter months, find creative ways to stay active. If the weather is too harsh for outdoor exercise, consider indoor activities such as:
Walking in a mall or indoor track
Joining a gym or fitness class
Practicing yoga or Pilates at home
Regular physical activity can help maintain cardiovascular fitness, reduce stress, and control weight.
Regularly check your blood pressure and cholesterol levels, especially during winter. If you have a history of high blood pressure or high cholesterol, work closely with your healthcare provider to manage these conditions effectively. Medications may need adjustments during colder months to ensure optimal control.
Nutrition plays a significant role in heart health. During winter, it's tempting to indulge in heavy, rich foods. Instead, focus on a balanced diet that includes:
Fruits and Vegetables: Aim for a variety of colorful fruits and vegetables, which provide essential vitamins, minerals, and antioxidants.
Whole Grains: Choose whole-grain options like brown rice, whole wheat bread, and quinoa for added fiber and nutrients.
Lean Proteins: Incorporate lean proteins such as fish, poultry, beans, and legumes to support muscle health without excess saturated fat.
Healthy Fats: Opt for healthy fats from sources like avocados, nuts, seeds, and olive oil, while limiting saturated and trans fats.
Although people tend to drink less water in winter, staying hydrated is crucial for heart health. Cold, dry air can lead to dehydration, which can strain the heart. Aim to drink plenty of fluids, even if you don't feel thirsty. Herbal teas, warm soups, and water-rich fruits and vegetables can help maintain hydration.
Winter can be a stressful time due to holiday obligations and shorter days. Engaging in stress-reducing activities is essential for heart health. Consider the following techniques:
Mindfulness and Meditation: Practices such as deep breathing, meditation, or yoga can help reduce stress levels.
Regular Social Interaction: Maintain connections with friends and family, as social support is vital for mental and emotional well-being.
Prioritize Sleep: Aim for 7-9 hours of quality sleep each night to support overall health and reduce stress.
Smoking significantly increases the risk of heart disease, and cold weather can exacerbate the harmful effects. If you smoke, seek support to quit. Additionally, be mindful of alcohol consumption, as excessive drinking can raise blood pressure and increase heart disease risk.
If you have a history of heart disease, be cautious when engaging in physical activities in cold weather. Avoid overexerting yourself, and listen to your body. If you feel fatigued or experience any warning signs, take a break and seek medical advice if necessary.
If you’re concerned about your heart health this winter, it’s essential to consult with an experienced cardiologist. At Felix Hospital, our team of expert cardiologists is dedicated to providing the best care and personalized treatment plans. Dr. Rahul Arora and Dr. Siddharth Samrat, both are the best cardiologists in Noida, specialize in diagnosing and treating various heart conditions. Don’t hesitate to reach out for expert advice on maintaining your heart health during the colder months.
If you have concerns about your heart health or want to learn more about treatment options, don’t hesitate to Click Here to contact Felix Hospital today!
As winter approaches, being proactive about heart health is more important than ever. Understanding the risks associated with cold weather and taking practical steps to protect your cardiovascular system can significantly reduce the chances of a heart attack. By dressing appropriately, staying active, eating a heart-healthy diet, managing stress, and seeking medical advice, you can navigate the winter months safely. Additionally, it's essential to consider the cost of heart attack treatment in Noida, ensuring you have access to quality care if needed. Remember, your heart health is a priority all year round.
1-Why does the risk of heart attacks increase in winter?
ANS: Cold temperatures cause blood vessels to constrict, raising blood pressure and increasing the heart's workload.
2-What are the warning signs of a heart attack?
ANS: Common symptoms include chest pain, shortness of breath, radiating pain, and other discomforts.
3-How can I stay active during the winter?
ANS: Consider indoor exercises, such as gym workouts, yoga, or walking in malls.
4-What should I eat to support heart health in winter?
ANS: Focus on fruits, vegetables, whole grains, lean proteins, and healthy fats.
5-Is it necessary to monitor blood pressure in winter?
ANS: Yes, especially for individuals with a history of high blood pressure or heart conditions.
6-What stress management techniques can I use?
ANS: Mindfulness, meditation, and social interactions can help reduce stress levels.
7-How much water should I drink during winter?
ANS: Aim for at least 8 glasses a day, adjusting based on activity levels and individual needs.
8-What role does smoking play in heart disease?
ANS: Smoking increases the risk of heart disease and should be avoided, especially in winter.
9-Who should I contact for heart health concerns?
ANS: Reach out to a cardiologist at a reputable hospital, such as Felix Hospital, for expert guidance.

Cold weather is commonly linked to seasonal illnesses such as the common cold and flu, but it can also significantly impact your heart health. As temperatures decline, the likelihood of heart attacks increases, particularly for those with pre-existing heart conditions. Although this may come as a surprise, cold weather can impose additional stress on the heart, heightening its vulnerability to heart attacks. Let’s delve into how cold weather affects heart health, the physiological changes it induces, and ways to safeguard yourself. For optimal treatment, consider searching for the best heart hospital in Noida.
Your well-being is our priority—take the first step towards a healthier heart today! Call us now at +91 9667064100.
A heart attack, or myocardial infarction, occurs when the blood flow to a part of the heart muscle is severely reduced or blocked. This blockage is typically caused by plaque buildup in the coronary arteries, a condition known as coronary artery disease. When the blood flow is restricted, the heart muscle doesn’t get the oxygen it needs, causing damage or death to part of the heart muscle. Immediate medical attention is crucial for survival and minimizing long-term damage.
Recognizing the symptoms of a heart attack is critical for prompt treatment. Common symptoms include:
Chest Pain or Discomfort: This is often described as pressure, squeezing, or fullness in the chest.
Shortness of Breath: Difficulty breathing can accompany chest pain or occur independently.
Nausea and Vomiting: Some individuals experience stomach discomfort or nausea.
Pain in the Arms, Neck, or Jaw: The pain may radiate from the chest to the upper body.
Cold Sweat: Sudden and profuse sweating is a common symptom.
Fatigue: Unexplained tiredness, especially in women, can indicate a heart attack.
If you or someone you know is experiencing these symptoms, seek emergency medical care immediately.
Cold weather presents unique challenges to the cardiovascular system. When exposed to cold temperatures, your body works harder to maintain its core temperature. This process increases the workload on your heart, which may already be strained in individuals with heart disease. The cold can cause your heart rate to rise and blood pressure to increase, both of which are risk factors for heart attacks. Additionally, cold weather is associated with increased levels of blood clotting, which can further heighten the risk of heart attacks by obstructing blood flow in the coronary arteries.
In response to cold weather, the body undergoes a process known as vasoconstriction, in which blood vessels narrow to conserve heat. While this mechanism is essential for keeping warm, it can also restrict blood flow and increase blood pressure. The reduced diameter of the blood vessels forces the heart to pump harder, placing additional strain on the cardiovascular system. For individuals with pre-existing heart conditions, this increased workload can trigger a heart attack or exacerbate symptoms of heart failure.
Yes, individuals with heart conditions such as coronary artery disease, heart failure, and arrhythmias are more vulnerable to the effects of cold weather. Those with coronary artery disease may experience chest pain (angina) more frequently due to the added strain on the heart. Heart failure patients may find it harder to breathe in cold air, while individuals with arrhythmias could notice irregular heartbeats. Even people without diagnosed heart conditions should be cautious in cold weather, as the added stress on the heart can lead to new heart problems.
Protecting your heart in cold weather requires proactive steps, especially if you are at higher risk for cardiovascular disease. Here are some essential tips to consider:
Dress Warmly: Wearing layers and covering your head, hands, and feet can help you stay warm and reduce the strain on your heart.
Stay Active Indoors: Cold weather can limit outdoor activities, but staying active indoors is crucial for maintaining heart health. Try light exercises such as walking in place, stretching, or yoga.
Monitor Your Blood Pressure: Keep an eye on your blood pressure, especially if you have hypertension or other heart-related conditions. Cold weather can cause spikes in blood pressure, increasing the risk of a heart attack.
Avoid Overexertion: Shoveling snow or engaging in strenuous activities in cold weather can put excessive strain on the heart. If you must do these activities, take frequent breaks, and don’t overdo it.
Stay Hydrated: Dehydration can thicken your blood, making it more likely to clot. Drink plenty of water, even when it’s cold outside.
Limit Alcohol Consumption: Alcohol can cause your body to lose heat more quickly and may lead to dehydration, increasing your heart’s workload.
Some individuals are more susceptible to cold-induced heart problems than others. Risk factors include:
Age: Older adults are more vulnerable to the effects of cold weather on heart health.
Pre-existing Heart Conditions: People with coronary artery disease, heart failure, or arrhythmias are at higher risk.
Hypertension: High blood pressure makes the heart work harder, especially in cold conditions.
Sedentary Lifestyle: Lack of physical activity can weaken the heart over time, making it more vulnerable to stress.
Smoking: Smoking damages the blood vessels and increases the risk of heart attacks, particularly in cold weather.
Obesity: Excess weight puts additional strain on the heart, and cold weather exacerbates this burden.
Preventing heart attacks during the winter months requires a combination of lifestyle changes and heart health awareness. Follow these prevention tips to reduce your risk:
Bundle Up: Dress warmly to prevent your body from losing heat and reduce the strain on your heart.
Exercise Regularly: Engage in regular cardiovascular exercise to strengthen your heart and improve circulation.
Eat a Heart-Healthy Diet: Consuming foods rich in omega-3 fatty acids, fiber, and antioxidants can help maintain heart health.
Quit Smoking: If you smoke, quitting is one of the most effective ways to reduce your risk of a heart attack.
Limit Salt and Alcohol: Both salt and alcohol can increase blood pressure, which is dangerous during cold weather.
Manage Stress: High stress levels can contribute to heart disease. Practice relaxation techniques like meditation or deep breathing exercises.
Get Regular Checkups: Visit your cardiologist for regular heart health checkups, especially during the winter months when the risk of heart attacks increases.
If you have concerns about your heart health or are experiencing symptoms that may indicate a heart condition, it’s important to consult with a specialist. At Felix Hospital, we have some of the best heart attack doctors in Noida who are experienced in diagnosing and treating a wide range of cardiovascular conditions Dr. Rahul Arora and Dr. Siddharth Samrat. Our cardiology team is committed to providing personalized care to help you maintain optimal heart health, especially during the colder months when the risk of heart attacks increases.
Cold weather can profoundly affect your heart health, elevating the risk of heart attacks, particularly among individuals with existing conditions. By gaining insight into how cold temperatures influence the cardiovascular system and adopting proactive measures to safeguard your heart, you can lower your risk significantly. If you're seeking expert cardiac care, Felix Hospital provides a range of comprehensive services to help maintain your heart's health throughout the year. Don’t wait for warning signs—make your heart health a priority today. For information on the costs of heart attack surgeries or treatments, visit the hospital.
1. Can cold weather trigger a heart attack?
ANS: Yes, cold weather can increase the risk of heart attacks by constricting blood vessels, raising blood pressure, and adding stress to the heart.
2. Who is most at risk for cold-weather heart attacks?
ANS: Older adults, individuals with heart disease, those with high blood pressure, smokers, and people who lead sedentary lifestyles are at higher risk.
3. Why do blood vessels constrict in cold weather?
ANS: The body constricts blood vessels to conserve heat, which helps maintain core body temperature but also increases blood pressure.
4. What should I do if I experience chest pain in the cold?
ANS: Seek emergency medical attention immediately if you experience chest pain, shortness of breath, or other symptoms of a heart attack.
5. How does high blood pressure contribute to heart attacks in cold weather?
ANS: Cold weather can cause blood pressure to rise, increasing the workload on the heart, which may lead to a heart attack in people with heart disease.
6. What can I do to prevent heart attacks in winter?
ANS: Dress warmly, avoid overexertion, maintain a healthy diet, quit smoking, and monitor your blood pressure to reduce your risk.
7. Can exercise in cold weather increase the risk of a heart attack?
ANS: Strenuous exercise in cold weather can increase the risk, especially if you have heart disease or are not used to physical activity.
8. Does alcohol affect heart health in the winter?
ANS: Yes, alcohol can cause heat loss, dehydration, and increased stress on the heart, raising the risk of heart problems in cold weather.
9. When should I see a cardiologist about cold-weather heart risks?
ANS: If you have heart disease, or high blood pressure, or experience symptoms such as chest pain or shortness of breath, see a cardiologist before winter begins to ensure you're taking the right precautions.

Congestive heart failure (CHF) is a chronic condition that affects millions of people worldwide, including a significant population in India. Heart failure occurs when the heart's ability to pump blood efficiently is compromised, leading to a buildup of fluid in the lungs, legs, and other organs. This article will explore the symptoms, stages, and causes of congestive heart failure, along with treatment options and associated costs. For those seeking effective care, choosing a specialized Congestive Heart Failure treatment Hospital can make a significant difference in managing this condition.
Contact Felix Hospital today to schedule a consultation with our experienced cardiologists. Your heart health is our priority. Call us at +91 9667064100.
Congestive heart failure (CHF) is a condition in which the heart muscles weaken and are unable to pump blood efficiently. This leads to inadequate circulation of blood and oxygen to vital organs, causing symptoms such as fatigue, shortness of breath, and fluid retention. CHF is often the result of underlying heart diseases such as coronary artery disease, high blood pressure, or heart attacks.
Left-sided heart failure: The left ventricle fails to pump blood effectively, causing blood to back up in the lungs.
Right-sided heart failure: The right ventricle fails, leading to fluid buildup in the legs, abdomen, and liver.
Heart failure is a progressive disease that worsens over time, making early detection and management crucial for improving the quality of life.
Congestive heart failure is classified into four stages based on the severity of symptoms and the heart’s ability to function:
Stage A: Pre-heart failure, where risk factors such as hypertension or diabetes are present, but there are no symptoms of heart failure.
Stage B: Structural heart disease is present, but the patient is still asymptomatic. This stage includes individuals with a previous heart attack or valve disease.
Stage C: The patient experiences symptoms such as shortness of breath, fatigue, and fluid retention due to structural heart disease.
Stage D: Advanced heart failure with severe symptoms despite optimal medical treatment, requiring advanced interventions such as heart transplant or palliative care.
The symptoms of congestive heart failure can vary depending on the stage of the disease. Common symptoms include:
Shortness of breath (dyspnea), especially during physical activities or while lying down
Fatigue and weakness
Swelling (edema) in the legs, ankles, and feet
Rapid or irregular heartbeat (palpitations)
Persistent cough or wheezing with white or pink-tinged phlegm
Increased need to urinate at night (nocturia)
Swelling of the abdomen due to fluid buildup (ascites)
Sudden weight gain from fluid retention
Decreased ability to exercise or engage in physical activities
Difficulty concentrating or mental confusion
If you experience any of these symptoms, it is essential to seek medical attention immediately.
Several factors can lead to congestive heart failure, including:
Coronary Artery Disease (CAD): The most common cause of CHF, CAD involves the narrowing or blockage of coronary arteries, reducing blood flow to the heart.
High Blood Pressure: Hypertension puts extra strain on the heart, weakening the muscles over time.
Heart Attack: A heart attack damages the heart muscle, reducing its ability to pump blood effectively.
Cardiomyopathy: Diseases of the heart muscle can cause it to become enlarged, thick, or rigid, impairing its function.
Valve Disease: Problems with the heart valves can lead to heart failure by disrupting the flow of blood within the heart.
Arrhythmias: Irregular heartbeats can reduce the heart's efficiency in pumping blood.
Diabetes: High blood sugar can damage blood vessels and increase the risk of heart failure.
Congenital Heart Defects: Some individuals are born with structural heart abnormalities that can lead to heart failure later in life.
Infections: Viral infections such as myocarditis can directly damage the heart muscle, leading to heart failure.
Diagnosing heart failure involves several steps, including a thorough medical history, physical examination, and various tests:
Electrocardiogram (ECG): Detects abnormal heart rhythms or evidence of a previous heart attack.
Echocardiogram: Uses sound waves to create images of the heart, showing its size, shape, and function.
Chest X-ray: Can reveal heart enlargement and fluid buildup in the lungs.
Blood Tests: To check for markers of heart failure, kidney function, and other health conditions.
Stress Test: Measures how well the heart works during physical exertion.
Coronary Angiography: A dye is injected into the coronary arteries to detect blockages or narrowing.
Early diagnosis is critical in managing heart failure effectively and preventing progression to advanced stages.
The treatment of congestive heart failure depends on the stage and severity of the condition. Common treatment approaches include:
ACE Inhibitors: Relax blood vessels and reduce blood pressure, making it easier for the heart to pump.
Beta-Blockers: Reduce heart rate and blood pressure, decreasing the heart's workload.
Diuretics: Help reduce fluid buildup in the body by increasing urine output.
Aldosterone Antagonists: Block the effects of hormones that cause salt and fluid retention.
Inotropes: Strengthen heart contractions in severe cases of heart failure.
Dietary Modifications: Reducing sodium intake and avoiding excessive fluid consumption can help manage fluid retention.
Exercise: Regular, moderate exercise can improve heart function and overall health.
Quitting Smoking: Smoking cessation is essential for reducing the risk of heart failure and other cardiovascular diseases.
Weight Management: Maintaining a healthy weight helps reduce the strain on the heart.
Coronary Bypass Surgery: This procedure restores blood flow to the heart by bypassing blocked coronary arteries.
Heart Valve Repair or Replacement: Damaged valves are either repaired or replaced to improve blood flow.
Implantable Cardioverter-Defibrillators (ICDs): These devices monitor heart rhythms and deliver shocks to correct dangerous arrhythmias.
Heart Transplant: In end-stage heart failure, a heart transplant may be necessary.
When considering these treatment options, it's essential to discuss the best Congestive Heart Failure treatment cost with your healthcare provider to ensure you receive the appropriate care within your budget.
Preventing heart failure involves managing risk factors and leading a heart-healthy lifestyle:
Control Blood Pressure: Keeping blood pressure within a healthy range is crucial to preventing heart damage.
Manage Diabetes: Proper diabetes management can reduce the risk of heart disease and heart failure.
Avoid Smoking: Smoking damages blood vessels and increases the risk of heart failure.
Exercise Regularly: Staying active helps maintain heart health and reduces the risk of obesity, hypertension, and other conditions.
Eat a Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can lower the risk of heart disease.
At Felix Hospital, we take pride in our team of dedicated and the best doctors for Congestive Heart Failure, including congestive heart failure. Our cardiologists, Dr. Rahul Aroral, Dr. Siddharth Samrat, are committed to providing personalized care and the latest treatment options to ensure the best possible outcomes for our patients. With their expertise and compassionate approach, we strive to deliver exceptional cardiac care tailored to meet each patient's unique needs.
Contact Felix Hospital today to book an appointment with the best cardiologists. Schedule a consultation by Clicking Here.
Congestive heart failure is a serious and progressive condition that requires timely diagnosis and intervention. With appropriate lifestyle changes, medication, and, in some cases, surgical treatments, patients with heart failure can manage their symptoms and improve their quality of life. Felix Hospital offers state-of-the-art cardiac care to ensure that you receive the best possible treatment for your heart health.
1-What is congestive heart failure (CHF)?
ANS: Congestive heart failure is a chronic condition where the heart cannot pump blood effectively, leading to fluid buildup in the lungs and other organs. This can result in symptoms such as shortness of breath, fatigue, and swelling.
2-What are the common symptoms of congestive heart failure?
ANS: Common symptoms include shortness of breath, fatigue, swelling in the legs and ankles, rapid or irregular heartbeat, persistent cough, and sudden weight gain due to fluid retention.
3-What are the main causes of congestive heart failure?
ANS: CHF can be caused by several factors, including coronary artery disease, high blood pressure, heart attacks, cardiomyopathy, valve disease, diabetes, and congenital heart defects.
4-How is congestive heart failure diagnosed?
ANS: Diagnosis typically involves a thorough medical history, physical examination, and tests such as electrocardiograms (ECG), echocardiograms, chest X-rays, and blood tests to assess heart function and identify underlying issues.
5-What are the stages of congestive heart failure?
ANS: CHF is classified into four stages:
Stage A: At risk but asymptomatic.
Stage B: Structural heart disease without symptoms.
Stage C: Symptoms present due to structural heart disease.
Stage D: Advanced heart failure with severe symptoms despite treatment.
6-What treatment options are available for congestive heart failure?
ANS: Treatment may include medications (such as ACE inhibitors, beta-blockers, and diuretics), lifestyle changes (like dietary modifications and exercise), and surgical options (such as valve repair, bypass surgery, or heart transplant).
7-Can lifestyle changes help manage congestive heart failure?
ANS: Yes, lifestyle changes such as reducing sodium intake, maintaining a healthy weight, quitting smoking, and engaging in regular physical activity can significantly improve heart health and manage CHF symptoms.
8-Is congestive heart failure a curable condition?
ANS: While CHF is generally not curable, it is manageable with appropriate treatments, lifestyle changes, and ongoing medical care. Many patients can lead fulfilling lives with effective management.
9-When should I seek medical attention for congestive heart failure symptoms?
ANS: You should seek medical attention if you experience worsening symptoms, such as increased shortness of breath, swelling, sudden weight gain, or severe fatigue. Early intervention is crucial for effective management.
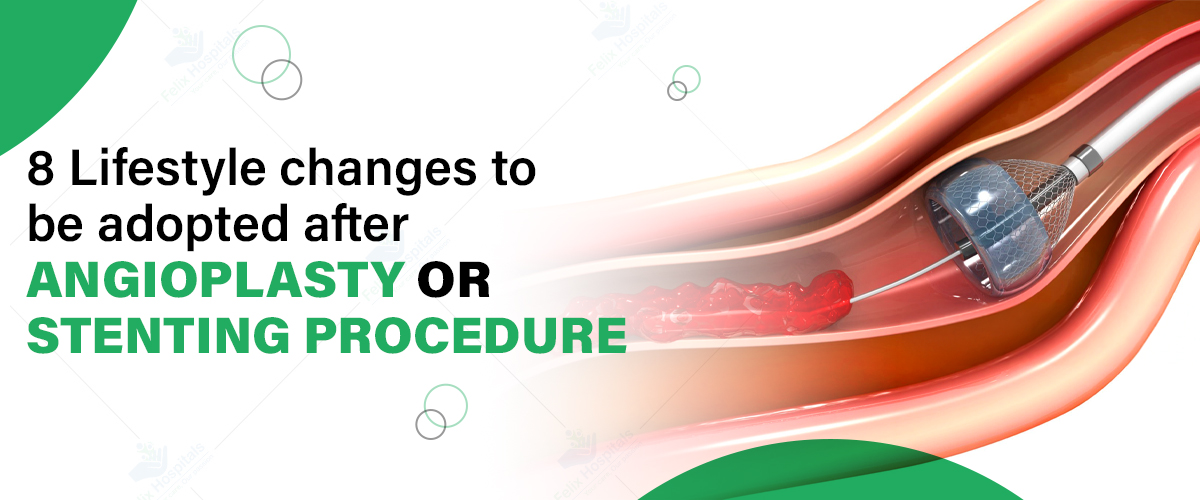
Angioplasty and stenting are common procedures performed to treat narrowed or blocked coronary arteries. They play a crucial role in restoring blood flow to the heart, ultimately reducing the risk of heart attacks and improving overall heart health. However, the journey doesn't end once the procedure is complete; significant lifestyle adjustments are necessary to ensure the long-term success of the treatment and to enhance overall well-being. Understanding the angioplasty surgery treatment cost and being proactive about heart health can significantly impact recovery and prevent further complications.
If you or a loved one has undergone angioplasty or stenting, it’s vital to take the next steps in your heart health journey. Schedule a consultation by Calling +91 9667064100.
Angioplasty is a minimally invasive surgical procedure used to open blocked or narrowed coronary arteries. During the procedure, a small balloon is inserted into the artery and inflated to widen it. In most cases, a stent (a small wire mesh tube) is placed in the artery to help keep it open and ensure proper blood flow.
This procedure is crucial for individuals suffering from coronary artery disease (CAD), as it helps alleviate symptoms such as chest pain (angina) and improves overall heart function. The goal of angioplasty surgery and stenting is to restore normal blood flow to the heart muscle, reducing the risk of serious heart conditions and enhancing the quality of life.
Recovering from angioplasty surgery or stenting involves making specific lifestyle changes to promote heart health. Here are eight essential changes to consider:
Importance: A balanced diet is foundational to promoting heart health. It not only helps in managing weight but also aids in controlling cholesterol and blood pressure levels, reducing the risk of future cardiovascular events.
Action: Aim to incorporate a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats into your daily meals. Reduce saturated fats, trans fats, sodium, and cholesterol intake, as these can contribute to arterial blockages.
Focus on foods rich in omega-3 fatty acids, such as fatty fish (like salmon and mackerel), walnuts, and flaxseeds, which can help lower triglyceride levels and reduce inflammation. Additionally, consider adopting a Mediterranean diet, known for its heart-healthy benefits, emphasizing olive oil, nuts, legumes, and whole grains.
Importance: Physical activity plays a crucial role in strengthening the heart, improving circulation, and maintaining a healthy weight. Regular exercise can also enhance your overall mood and energy levels.
Action: Aim for at least 150 minutes of moderate aerobic activity each week, which can include activities like brisk walking, cycling, or swimming. Start slowly and gradually increase the intensity and duration as your body adjusts.
Consult with your healthcare provider about safe exercise options tailored to your recovery stage. Incorporating strength training exercises a couple of times a week can also help improve muscle tone and support heart health.
Importance: Chronic stress can negatively impact heart health, leading to increased blood pressure and heart rate, which can exacerbate cardiovascular issues.
Action: Adopt effective stress management techniques such as mindfulness, meditation, yoga, or deep-breathing exercises. These practices can help calm the mind and body, reducing stress levels. Engaging in hobbies, spending time with loved ones, or participating in community activities can also provide emotional relief and contribute to a healthier lifestyle. Consider journaling or seeking professional counseling if stress becomes overwhelming.
Importance: Smoking is one of the most significant risk factors for heart disease, contributing to atherosclerosis (hardening of the arteries). Similarly, excessive alcohol consumption can lead to high blood pressure, irregular heartbeats, and other health complications.
Action: If you smoke, seek support to quit, whether through counseling, support groups, or nicotine replacement therapies. Limit alcohol intake to moderate levels—defined as up to one drink per day for women and up to two drinks per day for men. Staying within these guidelines can help protect your heart and overall health.
Importance: Maintaining a healthy weight is essential for heart health, as excess weight puts additional strain on the cardiovascular system and can lead to complications like hypertension and diabetes.
Action: Work towards achieving and maintaining a healthy weight through a combination of balanced eating and regular physical activity. Regularly track your weight and body mass index (BMI) to stay on course. If you find it challenging to lose weight, consider seeking the guidance of a registered dietitian or a nutritionist who can provide personalized meal planning and strategies tailored to your needs.
Importance: Following your prescribed medication regimen is critical for preventing further blockages and effectively managing heart health. Missing doses or discontinuing medications can increase the risk of serious complications.
Action: Take medications as directed by your healthcare provider, and keep a medication schedule to ensure that doses are not missed. Utilize pill organizers or mobile apps to help track your medications. It's essential to communicate with your doctor about any side effects or concerns you may experience. Regularly reviewing your medications with your healthcare provider can also help optimize your treatment plan.
Importance: Regular follow-ups with your healthcare provider can help monitor your recovery and detect any potential issues early, ensuring that any concerns are addressed promptly.
Action: Schedule regular check-ups and necessary tests, such as blood pressure and cholesterol screenings, to ensure that your heart health remains stable. Discuss any new symptoms or changes in your health with your healthcare provider during these visits. Staying proactive about your health can make a significant difference in your recovery and long-term well-being.
Importance: Understanding your condition and treatment options empowers you to make informed decisions about your health. Being well-informed helps you recognize symptoms early and understand the importance of lifestyle changes.
Action: Stay updated on heart health information and research through reputable sources. Consider participating in support groups or educational programs that connect you with others who have undergone similar procedures. Engaging with healthcare professionals and seeking knowledge about your heart condition can foster a sense of control and encourage you to adhere to a heart-healthy lifestyle.
At Felix Hospital, we pride ourselves on having a team of highly qualified cardiologists dedicated to providing exceptional care. If you're looking for the best doctor for angioplasty surgery, consider consulting with our experienced cardiologists who specialize in heart health and recovery. Among them are Dr. Rahul Arora, Dr. Siddharth Samrat, each committed to supporting your journey to better heart health after your angioplasty surgery or stenting procedure.
For personalized advice and guidance on managing your heart health after angioplasty, book an appointment with our expert cardiologists today by Clicking Here!
Living a heart-healthy lifestyle is crucial after undergoing angioplasty surgery or stenting. By adopting these eight lifestyle changes, you can improve your overall health and significantly reduce the risk of future heart-related issues. Remember that recovery is a journey, and staying proactive about your health will lead to a more fulfilling life. Moreover, understanding the angioplasty surgery treatment cost will enable you to make informed decisions regarding your healthcare options.
1-What is angioplasty, and how does it work?
ANS: Angioplasty is a procedure to open blocked or narrowed coronary arteries using a balloon and often a stent to maintain blood flow.
2-What are the typical recovery times after angioplasty?
ANS: Recovery times vary, but most people can return to normal activities within a week. Full recovery may take several weeks.
3-How can I prevent the recurrence of coronary artery disease?
ANS: By adopting a heart-healthy lifestyle, managing risk factors, and adhering to your treatment plan, you can reduce the risk of recurrence.
4-Is it necessary to change my diet after angioplasty?
ANS: Yes, a heart-healthy diet is crucial for recovery and long-term heart health.
5-What types of exercise are safe after angioplasty?
ANS: Low-impact exercises such as walking, cycling, and swimming are generally safe. Always consult your doctor before starting a new exercise regimen.
6-How often should I have check-ups after angioplasty?
ANS: Follow-up appointments should be scheduled regularly, usually at least once a year, or more frequently if advised by your doctor.
7-Can I still take over-the-counter medications after angioplasty?
ANS: Consult your doctor before taking any over-the-counter medications to ensure they do not interfere with your prescribed treatment.
8- What should I do if I experience symptoms after the procedure?
ANS: Contact your healthcare provider immediately if you experience chest pain, shortness of breath, or any unusual symptoms following your procedure.

Cardiovascular conditions are a leading cause of death worldwide, and two of the most dangerous heart-related emergencies are sudden cardiac arrest (SCA) and heart attacks. While both affect the heart, they are distinct conditions with different causes, symptoms, and treatments. Understanding these differences is crucial, as prompt treatment can be life-saving in both situations. If you're looking for heart care, the Best Cardiology Hospital is your trusted partner in managing and treating heart emergencies with precision and expertise.
Let’s dive into the differences between sudden cardiac arrest and heart attacks, explore their signs and symptoms, and understand what causes these potentially life-threatening events.
Learn more about the signs and symptoms, and find out how you can take proactive steps toward prevention. Contact us today at +91 9667064100.
A heart attack, medically known as a myocardial infarction, occurs when the blood flow to a section of the heart muscle becomes blocked. This blockage is often caused by a buildup of plaque (a mixture of fat, cholesterol, and other substances) in the coronary arteries, which supply blood to the heart. When the plaque ruptures, a blood clot forms, restricting or completely blocking the flow of oxygen-rich blood to the heart muscle. Without a sufficient blood supply, the heart muscle begins to die, leading to a heart attack.
The symptoms of a heart attack can vary from person to person, but common signs include:
1. Chest pain or discomfort: A common symptom is pain or discomfort in the center or left side of the chest, which may feel like pressure, squeezing, fullness, or pain. It can last for several minutes or come and go.
2. Discomfort in other areas of the upper body: Pain or discomfort may also spread to the shoulders, arms, back, neck, jaw, or stomach.
3. Shortness of breath: Difficulty breathing often accompanies chest pain and can happen before or during a heart attack.
4. Cold sweat: Excessive sweating, especially when not exerting yourself physically, can be a sign of a heart attack.
5. Fatigue: Feeling unusually tired without a clear cause may indicate a heart issue, especially in women.
6. Nausea, vomiting, or lightheadedness: Some individuals, particularly women, may experience these symptoms during a heart attack.
Heart attacks are primarily caused by coronary artery disease (CAD), a condition where the arteries that supply blood to the heart become narrow or blocked due to plaque buildup. Other contributing factors include:
Smoking
High cholesterol levels
High blood pressure
Obesity
Lack of physical activity
Diabetes
Unhealthy diet
Stress
Family history of heart disease
Sudden cardiac arrest (SCA) is a medical emergency that occurs when the heart suddenly stops beating due to an electrical malfunction. This leads to an immediate cessation of blood flow to the brain, lungs, and other vital organs. Without prompt intervention, sudden cardiac arrest can be fatal within minutes. Unlike a heart attack, SCA does not involve blocked arteries but is usually caused by electrical disturbances in the heart that disrupt its pumping action.
The symptoms of sudden cardiac arrest are abrupt and severe, often occurring without warning. Common signs include:
1. Sudden collapse: The most noticeable symptom is a sudden loss of consciousness and collapse, with no warning signs.
2. No pulse: Because the heart has stopped beating, there is no detectable pulse.
3. No breathing: Victims of sudden cardiac arrest stop breathing or have abnormal breathing (gasping or struggling for breath).
4. Loss of consciousness: The person becomes unresponsive immediately.
Sudden cardiac arrest is typically caused by electrical disturbances in the heart. The most common cause is a condition known as ventricular fibrillation, where the heart’s lower chambers quiver instead of pumping blood. Other causes include:
Coronary artery disease: SCA is often linked to coronary artery disease, where plaque buildup in the arteries can trigger electrical issues.
Heart attack: A heart attack can trigger sudden cardiac arrest by damaging the heart’s electrical system.
Arrhythmias: Abnormal heart rhythms, especially ventricular tachycardia and fibrillation, increase the risk of SCA.
Congenital heart conditions: Individuals born with certain heart defects are at higher risk for sudden cardiac arrest.
Heart failure: Weakening of the heart muscle due to chronic conditions can lead to SCA.
Hypertrophic cardiomyopathy: A condition where the heart muscle becomes abnormally thick, making it harder for the heart to pump blood and increasing the risk of SCA.
While both SCA and heart attacks are life-threatening emergencies involving the heart, they are distinctly different conditions:
1. Cause:
A heart attack is caused by a blocked artery that prevents blood flow to a part of the heart.
Sudden cardiac arrest is caused by an electrical malfunction in the heart that causes it to stop beating effectively.
2. Symptoms:
Heart attack symptoms often develop gradually over time, with warning signs such as chest pain, shortness of breath, and discomfort in other parts of the body.
Sudden cardiac arrest occurs without warning, and the person typically loses consciousness immediately.
3. Outcome:
A heart attack, if treated promptly, may leave the heart damaged but still functioning.
Sudden cardiac arrest is fatal unless immediate treatment is provided, such as CPR or defibrillation.
4. Connection:
A heart attack can sometimes lead to sudden cardiac arrest, especially if the heart’s electrical system is damaged during the attack.
Diagnosing a heart attack requires urgent medical attention. Common diagnostic tests include:
Electrocardiogram (ECG): Measures the heart’s electrical activity and can detect abnormalities caused by a heart attack.
Blood tests: Blood tests can detect markers such as troponins, which are released when the heart muscle is damaged.
Coronary angiography: This imaging test uses contrast dye and X-rays to visualize the coronary arteries and detect blockages.
In cases of sudden cardiac arrest, diagnosis occurs in the emergency room, as the focus is on reviving the patient. Key diagnostic tools include:
ECG: Used to detect abnormal heart rhythms.
Echocardiogram: Uses sound waves to create images of the heart to check for structural issues.
Blood tests: Help determine if any underlying conditions, such as heart attacks, triggered the event.
The treatment for a heart attack focuses on restoring blood flow to the heart. Common treatments include:
1. Medications: Blood thinners, clot-busting drugs, and pain relievers are often administered to break up clots and alleviate symptoms.
2. Angioplasty and stenting: A procedure where a balloon is inserted into the blocked artery to open it, often followed by placing a stent to keep the artery open.
3. Coronary artery bypass grafting (CABG): Surgery where blood vessels from other parts of the body are used to bypass blocked arteries.
Immediate treatment for SCA focuses on restoring a normal heart rhythm. The primary life-saving interventions include:
1. Cardiopulmonary resuscitation (CPR): Quick, hard chest compressions can help maintain blood flow to the brain and other organs until emergency help arrives.
2. Defibrillation: An automated external defibrillator (AED) delivers an electric shock to the heart to restore its normal rhythm.
3. Implantable cardioverter defibrillator (ICD): For people at high risk of SCA, an ICD can be implanted to monitor and correct abnormal heart rhythms.
Coronary artery disease
High blood pressure
Smoking
High cholesterol
Diabetes
Family history of heart disease
Obesity
Sedentary lifestyle
Prior history of heart attack
Arrhythmias
Congenital heart defects
Heart failure
Preventing heart attacks and sudden cardiac arrest often involves making healthy lifestyle changes. Key preventive measures include:
Healthy diet: A diet rich in fruits, vegetables, whole grains, and lean proteins can help manage cholesterol and blood pressure levels.
Regular exercise: Engaging in physical activity for at least 150 minutes a week improves heart health.
Quit smoking: Smoking is a major risk factor for heart disease and should be avoided.
Manage stress: Chronic stress can increase the risk of heart attacks and cardiac events.
Control underlying conditions: Properly managing diabetes, hypertension, and high cholesterol is crucial to reducing the risk of heart disease.
Dr. Rahul Arora, Dr. Siddharth Samrat, With their extensive experience and expertise in cardiology, these specialists are dedicated to providing top-notch heart care. From diagnosing complex cardiovascular conditions to delivering personalized treatment plans, they are committed to helping patients achieve optimal heart health. Trust our team of the Best cardiologists in Noida for compassionate care and cutting-edge solutions tailored to your needs.
Book your consultation by Clicking Here now to stay heart-healthy and prevent life-threatening conditions. Protect Your Heart Today!
Understanding the differences between sudden cardiac arrest and heart attack is essential for taking quick and appropriate action during a cardiac emergency. While both conditions can be life-threatening, recognizing the signs, seeking immediate medical care, and adopting heart-healthy lifestyle changes can greatly reduce the risk of these cardiovascular events. Additionally, being informed about the heart treatment cost in Noida allows patients to seek timely care without unnecessary delays, ensuring the best possible outcomes for heart-related emergencies.
1. What is the difference between a heart attack and sudden cardiac arrest?
ANS: A heart attack occurs when blood flow to the heart is blocked, while sudden cardiac arrest happens when the heart's electrical system malfunctions and the heart suddenly stops beating.
2. What are the warning signs of a heart attack?
ANS: Common symptoms include chest pain, discomfort in other areas like the arms or jaw, shortness of breath, cold sweat, fatigue, and nausea.
3. Can a heart attack lead to sudden cardiac arrest?
ANS: Yes, a heart attack can sometimes cause electrical disturbances in the heart, which can lead to sudden cardiac arrest, especially if the heart muscle is severely damaged.
4. What should I do if someone is experiencing sudden cardiac arrest?
ANS: Call emergency services immediately. Perform CPR and use an automated external defibrillator (AED) if available until professional help arrives.
5. Who is at higher risk for heart attacks and sudden cardiac arrest?
ANS: Individuals with coronary artery disease, high blood pressure, high cholesterol, diabetes, a family history of heart disease, or unhealthy lifestyle habits (such as smoking) are at greater risk.
6. How can I prevent heart attacks and sudden cardiac arrest?
ANS: Leading a healthy lifestyle—exercising regularly, eating a balanced diet, quitting smoking, managing stress, and controlling medical conditions like hypertension and diabetes—can significantly reduce the risk.
7. What are the treatment options for a heart attack?
ANS: Treatment options include medications, angioplasty, stenting, or coronary artery bypass surgery to restore blood flow to the heart.
8. Is sudden cardiac arrest always fatal?
ANS: Sudden cardiac arrest is fatal if not treated immediately, but quick action with CPR and defibrillation can save lives. Early recognition of symptoms and immediate treatment are critical.
A cardiac stress test is a valuable diagnostic tool used to assess the heart's response to physical exertion or stress. It helps healthcare providers determine how well the heart functions during increased activity levels and can reveal underlying heart conditions that may not be evident at rest. This test is especially important for individuals with risk factors for heart disease and stress tests, those experiencing chest pain, or anyone undergoing preoperative evaluations. If you're seeking a Cardiac Stress Test hospital, it's crucial to choose a facility with experienced professionals who can guide you through the process. Let’s explore the different types of cardiac stress tests, how long they typically last, associated risks and side effects, the procedure itself, and the treatment costs involved.
If you’re experiencing symptoms such as chest pain, shortness of breath, or fatigue, don’t hesitate to reach out for professional help. Contact Felix Hospital at +91 9667064100.
A cardiac stress test measures how well your heart works under physical stress. It typically involves exercising on a treadmill or stationary bike while monitoring heart rate, blood pressure, and electrocardiogram (ECG) readings. The test can help identify issues such as coronary artery disease, arrhythmias, and other heart-related conditions. In some cases, if a patient is unable to exercise, medications may be administered to simulate the effects of exercise on the heart.
Cardiac stress tests come in various forms, each tailored to assess heart function and health under specific conditions. Understanding these different types can help you and your healthcare provider choose the most appropriate test for your situation. Here’s a more detailed look at each type:
Treadmill Stress Test: This is the most commonly performed cardiac stress test. During this test, patients walk on a treadmill, starting at a slow pace and gradually increasing the intensity. The treadmill’s incline and speed are adjusted based on a specific protocol, allowing the heart to be monitored continuously throughout the exercise. This test is particularly effective in evaluating exercise capacity and identifying any ischemic changes in the heart's electrical activity that may occur with increased physical exertion.
Exercise Bike Stress Test: Similar to the treadmill stress test, this procedure involves pedaling a stationary bike. The resistance on the bike is gradually increased, allowing healthcare professionals to monitor the heart's response to increased physical demand. This test can be more comfortable for patients who may have balance issues or difficulty walking, as it allows for a seated position while still providing valuable information about heart function.
Nuclear Stress Test: This advanced test provides detailed images of the heart’s blood flow. A small amount of radioactive material is injected into the bloodstream before and after the exercise phase. This allows doctors to visualize blood flow to the heart muscle using a special camera. By comparing images taken at rest and during stress, the test can help identify areas of the heart that may not be receiving adequate blood supply, indicating potential blockages in the coronary arteries.
Stress Echocardiogram: This test combines the principles of echocardiography with a stress test. It involves taking ultrasound images of the heart before and after exercise. The patient undergoes a treadmill or exercise bike test, and echocardiographic images are captured during different phases of the test. This dual approach provides real-time insight into the heart's structure and function under stress, helping identify abnormalities in heart motion, which can be indicative of coronary artery disease.
Pharmacologic Stress Test: For patients who are unable to exercise due to physical limitations or health conditions, a pharmacologic stress test may be utilized. In this test, medications are administered to stimulate the heart, mimicking the effects of exercise. These medications increase heart rate and induce a stress response while patients are monitored closely. Imaging techniques such as echocardiography or nuclear imaging can be used alongside this test to assess heart function.
The duration of a cardiac stress test varies depending on several factors, but the entire process typically takes between 30 to 60 minutes. This timeframe includes preparation, the actual test, and the recovery period.
Preparation: Before the test begins, you will be asked to change into a hospital gown and have electrodes placed on your chest to monitor your heart activity. This setup may take about 10 to 15 minutes. It’s essential to provide your medical history, including any medications you’re currently taking, as this can influence the test.
Exercise Portion: The actual exercise segment of the stress test may last anywhere from 5 to 15 minutes. The length can vary based on the type of test and your physical capacity. For instance, during a treadmill test, the goal is to reach a target heart rate based on your age and fitness level, and the duration will depend on how quickly you reach that target.
Recovery Phase: After completing the exercise component, you will enter a recovery phase. During this time, your heart rate, blood pressure, and ECG will continue to be monitored as your body returns to its resting state. This phase can last anywhere from 10 to 20 minutes, allowing healthcare professionals to ensure that your heart is stabilizing properly after exertion.
While cardiac stress tests are generally safe, there are some risk factors to consider:
Heart Conditions: Patients with known heart problems may have a higher risk during the test.
Respiratory Issues: Conditions such as asthma or chronic obstructive pulmonary disease (COPD) can complicate the test.
Blood Pressure Issues: Individuals with low or high blood pressure should inform their healthcare provider beforehand.
Medications: Certain medications may affect heart function and should be discussed with a physician before testing.
While side effects from a cardiac stress test are rare, some patients may experience:
Fatigue: Due to physical exertion, fatigue may occur during or after the test.
Chest Discomfort: Some patients may experience mild chest pain or discomfort during exercise.
Shortness of Breath: This can happen, particularly if the individual has pre-existing respiratory conditions.
Dizziness or Nausea: Some individuals may feel dizzy or nauseous, especially if they exert themselves significantly.
Here’s what you can expect during a cardiac stress test:
1. Preparation: You’ll be asked to change into a hospital gown and may need to refrain from eating, drinking, or smoking for a few hours before the test.
2. Baseline Measurements: Medical staff will record your baseline heart rate, blood pressure, and ECG readings before you start exercising.
3. Exercise Phase: You will begin exercising on a treadmill or stationary bike. The intensity will gradually increase, with staff monitoring your vital signs throughout.
4. Monitoring: During the test, medical professionals will continuously monitor your heart rate, blood pressure, and ECG to assess your heart’s response to stress.
5. Recovery Phase: After reaching your target heart rate or if you experience significant symptoms, the test will stop. You’ll be allowed to rest, and your heart will be monitored as it returns to its normal state.
6. Post-Test Evaluation: Once you’ve recovered, the medical team will analyze your test results and discuss them with you.
The cost of a cardiac stress test can vary significantly based on several factors, including the type of test performed, the facility where the test is conducted, and any additional services or imaging required. Generally, standard treadmill or exercise bike stress tests may be more affordable. In contrast, more specialized tests, such as nuclear stress tests or stress echocardiograms, involve advanced imaging and materials that can increase the overall cost. Additionally, patients can consider a healthy heart package that may bundle several cardiac assessments, including stress tests, at a reduced rate. Insurance coverage plays a crucial role in determining out-of-pocket expenses, with many plans covering a portion of the costs if the test is deemed medically necessary. Patients should consult their healthcare provider and insurance company to obtain a detailed estimate tailored to their situation.
At Felix Hospital, we pride ourselves on having some of the best Doctors for cardiac stress tests in Noida:
Dr. Rahul Arora: An experienced cardiologist specializing in various heart conditions, Dr. Arora is dedicated to providing comprehensive cardiac care.
Dr. Siddharth Samrat: With years of expertise, Dr. Samrat focuses on innovative diagnostic and treatment methods, ensuring the best possible outcomes for his patients.
Don’t leave your heart health to chance. Contact Felix Hospital today Click Here to schedule your cardiac stress test or consultation with our top cardiologists.
A cardiac stress test is an essential tool for assessing heart health and function. Understanding the types, duration, risks, side effects, and procedures involved can help you feel more prepared and informed. With the expertise of leading cardiologists at Felix Hospital, you can receive the highest quality care tailored to your needs. Consider a full heart checkup in Noida to comprehensively evaluate your heart health. Prioritize your heart health today and take the first step towards a healthier future.
1. What is a cardiac stress test?
ANS: A cardiac stress test evaluates how well your heart functions under physical stress. It typically involves exercise, like walking on a treadmill or pedaling a stationary bike, while monitoring heart rate, blood pressure, and ECG.
2. Who needs a cardiac stress test?
ANS: Cardiac stress tests are often recommended for individuals experiencing symptoms such as chest pain, shortness of breath, or abnormal heart rhythms. They may also be used for those with a history of heart disease and stress tests or to assess exercise capacity before starting a new exercise program.
3. How should I prepare for a cardiac stress test?
ANS: Preparation may include avoiding caffeine, smoking, and certain medications 24 hours before the test. You should wear comfortable clothing and shoes suitable for exercise. Your healthcare provider will give specific instructions tailored to your situation.
4. What should I expect during the test?
ANS: During the test, you'll be monitored closely as you exercise. You may feel some fatigue or shortness of breath, which is expected. The healthcare team will assess your heart's response to the exercise and may stop the test if necessary for your safety.
5. Are there any risks associated with a cardiac stress test?
ANS: While generally safe, potential risks include abnormal heart rhythms, chest pain, or, in rare cases, heart attack. Your healthcare provider will evaluate your medical history to minimize risks before the test.
6. What are the side effects of a cardiac stress test?
ANS: Some common side effects may include fatigue, lightheadedness, or muscle soreness after the exercise. Most patients recover quickly, and any discomfort usually subsides shortly after the test.
7. How long does it take to get results from a cardiac stress test?
ANS: Results can typically be discussed with your healthcare provider shortly after the test, but detailed analysis may take a few days. Your provider will explain the findings and recommend any necessary follow-up.
8. Where can I get a cardiac stress test?
ANS: Cardiac stress tests are available at specialized cardiac clinics, hospitals, and outpatient centers. At Felix Hospital, our experienced cardiologists, including Dr. Rahul Arora, Dr. Siddharth Samrat, and Dr. Syed Zafrul Hasan, provide comprehensive cardiac care and testing.
MBBS, MD Physician, PGDCC
Over his 13+ years of experience, Dr. Virendra Singh is a highly experienced Clinical Cardiologist dedicated to delivering comprehensive care for a broad spectrum of cardiovascular conditions. He specializes in the diagnosis and management of heart diseases, with a focus on creating personalized, patient-centered treatment plans. Dr. Singh's expertise includes conducting non-invasive diagnostic tests such as echocardiograms, stress tests, and advanced cardiac imaging to ensure accurate assessments. He is adept at managing complex cardiovascular cases, including critically ill patients, and is committed to using evidence-based approaches to improve patient outcomes.
Education
Areas Of Interest
Previous Experiences
Awards and Achievements:
Achieved Professional Qualification as a cardiologist from the Indra Gandhi National Open University.
Language