
Subscribe to our
ह्यूमन मेटान्यूमोवायरस (एचएमपीवी) एक श्वसन वायरस है जो मानव श्वसन तंत्र को प्रभावित करता है। इसे पहली बार 2001 में पहचाना गया था और यह पैरामाइक्सोविरिडे परिवार से संबंधित है। यह वायरस विशेष रूप से बच्चों, बुजुर्गों और कमजोर प्रतिरक्षा प्रणाली वाले लोगों के लिए गंभीर स्वास्थ्य समस्याएं पैदा करता है। एचएमपीवी कोई नया वायरस नहीं है। यह 2023 में चीन अमेरिका, नीदरलैंड, ब्रिटेन और अन्य देशों में भी देखा गया था। भारत में यह सामान्य मौसमी संक्रमणों के रूप में ही रहता है। इसलिए घबराने की जरूरत नहीं है, बल्कि सतर्कता बरतनी चाहिए।
ज्यादा जानकारी के लिए हमें कॉल करें +91 9667064100।
एचएमपीवी क्या है ? (What is HMPV?)
बच्चों में एचएमपीवी के लक्षण (Symptoms of HMPV in children)
बुजुर्गों में एचएमपीवी के लक्षण (Symptoms of HMPV in the elderly)
इलाज और प्रबंधन (Treatment and management)
फेलिक्स हॉस्पिटल्स में एचएमपीवी विशेषज्ञ के बारे में जानें (Know the Specialist for HMPV in Felix Hospitals)
निष्कर्ष (Conclusion)
अक्सर पूछे जाने वाले सवाल और जवाब ( Frequently asked questions and answers)
एचएमपीवी एक श्वसन वायरस है, जो मुख्य रूप से फेफड़ों और श्वसन तंत्र को प्रभावित करता है। यह वायरस बच्चों, वृद्ध लोगों और कमजोर प्रतिरक्षा प्रणाली वाले व्यक्तियों के लिए अधिक जोखिमपूर्ण हो सकता है। यह ऊपरी और निचले श्वसन तंत्र में संक्रमण का कारण बनता है। इसके कारण ब्रोंकाइटिस और निमोनिया जैसे लक्षण दिखते हैं। एचएमपीवी संक्रमित व्यक्ति के शारीरिक द्रवों के संपर्क से फैलता है जैसे खांसी और छींक से निकलने वाली बूंदें। संक्रमित सतहों को छूने के बाद हाथ, मुंह या नाक को छूना। संक्रमित व्यक्ति के निकट संपर्क में आने से भी फैलता है।
1. सामान्य लक्षण:
बुखार
खांसी
नाक बहना
2. श्वसन समस्याएं:
घरघराहट
सांस लेने में कठिनाई
3. गंभीर संक्रमण:
निमोनिया
ब्रॉन्कियोलाइटिस
ज्यादा जोखिम किसे होता है ?
जन्मजात बीमारियों वाले बच्चे: जिन बच्चों में जन्म से ही हृदय या फेफड़ों की बीमारी हो।
अस्थमा या एलर्जी वाले बच्चे: जिन्हें पहले से सांस की बीमारियां हों।
कमजोर इम्यूनिटी वाले बच्चे: जिनकी रोग प्रतिरोधक क्षमता कमजोर है।
6 महीने से छोटे बच्चे: छोटे बच्चों में एचएमपीवी से लड़ने की क्षमता कम होती है।
1. सामान्य लक्षण:
खांसी
सांस फूलना (डिस्प्निया)
गले में खराश
नाक बहना या जाम होना
बुखार और ठंड लगना
2. गंभीर लक्षण:
अत्यधिक थकान और कमजोरी
सीने में जकड़न या दर्द
ऑक्सीजन का स्तर कम होना (हाइपोक्सिया)
तेज़ या कठिन सांस लेना
3. कठिनाई:
निमोनिया (फेफड़ों में संक्रमण)
ब्रोन्काइटिस
फेफड़ों और हृदय की पुरानी समस्याओं का बिगड़ना
उच्च जोखिम वाले समूह:
60 वर्ष से अधिक उम्र के लोग
फेफड़ों और हृदय की पूर्व समस्याओं वाले मरीज (जैसे सीओपीडी, अस्थमा, या हृदय रोग)
कमजोर प्रतिरक्षा प्रणाली वाले लोग (जैसे डायबिटीज, कैंसर उपचार से गुजर रहे लोग, या ट्रांसप्लांट मरीज़)
1. लक्षणों के आधार पर उपचार:
बुखार और दर्द कम करना: डॉक्टर की सलाह पर पैरासिटामोल या अन्य बुखार कम करने वाली दवाओं का उपयोग करें।
तरल पदार्थ की आपूर्ति: शरीर को हाइड्रेट रखने के लिए पर्याप्त पानी, जूस और सूप का सेवन करें। गंभीर मामलों में तरल की कमी को दूर करने के लिए ड्रिप लगाई जा सकती है।
खांसी और गले की खराश: गर्म पानी से गरारे करें। खांसी कम करने के लिए हल्दी वाला दूध या अदरक-शहद का सेवन करें।
2. गंभीर मामलों में चिकित्सा सहायता:
ऑक्सीजन थेरेपी: यदि ऑक्सीजन का स्तर कम हो तो ऑक्सीजन सपोर्ट की आवश्यकता हो सकती है।
वेंटिलेटर सपोर्ट: श्वसन फेलियर के मामलों में वेंटिलेटर की जरूरत पड़ सकती है।
हॉस्पिटलाइजेशन: निमोनिया, हाइपोक्सिया या ब्रोन्काइटिस के मामलों में अस्पताल में भर्ती होना अनिवार्य हो सकता है।
3. डॉक्टर से कब संपर्क करें ?
सांस लेने में कठिनाई (डिस्प्निया)।
सीने में जकड़न या दर्द।
गंभीर खांसी या बलगम में खून आना।
अत्यधिक सुस्ती या कमजोरी।
बच्चा खाना पीना बंद कर दे या तेज सांस ले।
4. अतिरिक्त सुझाव:
व्यक्तिगत स्वच्छता का महत्व
>हाथ धोना: साबुन और पानी से कम से कम 20 सेकंड तक हाथ धोएं। यदि पानी उपलब्ध न हो, तो अल्कोहल-आधारित सैनिटाइजर का उपयोग करें।
>मास्क पहनना: भीड़भाड़ वाले स्थानों या संक्रमित व्यक्ति के पास जाते समय मास्क पहनें।
बच्चों और बुजुर्गों का विशेष ध्यान:
उन्हें भीड़भाड़ वाले स्थानों, जैसे बाजार, सार्वजनिक परिवहन और सामूहिक कार्यक्रमों में जाने से बचाएं। स्कूल या अन्य संस्थानों में बच्चों को शारीरिक दूरी और स्वच्छता का महत्व समझाएं।
संक्रमित व्यक्ति से दूरी बनाए रखना:
संक्रमित व्यक्ति के संपर्क से बचें। उनके उपयोग किए गए कपड़े, बर्तन या अन्य वस्तुओं को छूने के बाद तुरंत हाथ धोएं। यदि परिवार का कोई सदस्य संक्रमित है, तो उनके लिए अलग कमरे और व्यक्तिगत वस्तुओं का उपयोग सुनिश्चित करें।
प्रतिरक्षा प्रणाली को मजबूत करना
पोषणयुक्त आहार: ताजे फल और सब्जियां (विटामिन सी और जिंक युक्त) जैसे संतरा, आंवला, और पालक का सेवन। प्रोटीन युक्त खाद्य पदार्थ, जैसे दाल, अंडे और नट्स का सेवन करें।
भरपूर पानी पीना: दिनभर हाइड्रेटेड रहें।
व्यायाम और योग: नियमित व्यायाम और ध्यान प्रतिरक्षा को मजबूत करने में मदद करता है।
पर्याप्त नींद: प्रतिरक्षा प्रणाली को दुरुस्त रखने के लिए 7-8 घंटे की पर्याप्त नींद लें।
एचएमपीवी संक्रमण के कारण फेफड़ों पर असर पड़ने पर हमारे विशेषज्ञ आपकी देखभाल के लिए तत्पर हैं। श्वसन तंत्र की समस्याओं जैसे सांस फूलना, निमोनिया और ब्रोन्काइटिस के निदान और उपचार के लिए डॉ. प्रियदर्शी जितेंद्र कुमार, जो सबसे अनुभवी पल्मोनोलॉजिस्ट हैं, का नेतृत्व करते हुए हमारी कुशल टीम आपकी सेवा में है।
साथ ही, हमारी जनरल फिजिशियन विशेषज्ञों की टीम में शामिल हैं डॉ. अंशुमाला सिन्हा, डॉ. सोनाक्षी सक्सेना, डॉ. अपूर्वा शेट्टी, डॉ. नीलाभ प्रताप, डॉ. प्रियंका सिंह, डॉ. रवि शर्मा, और डॉ. केशव कुमार गर्ग। फेलिक्स हॉस्पिटल पर भरोसा करें, जहां विशेषज्ञता और समर्पण दोनों हैं।
डॉक्टर की सलाह के लिए आज ही फोन करें +91 9667064100 और अपना अपॉइंटमेंट बुक करें।
एचएमपीवी के खिलाफ सतर्कता और जागरूकता से संक्रमण को नियंत्रित किया जा सकता है। सही समय पर कार्रवाई, स्वच्छता, और स्वास्थ्यप्रद आदतों का पालन संक्रमण से बचाव का सबसे प्रभावी तरीका है। अपने और अपने परिवार के स्वास्थ्य का ध्यान रखें और किसी भी श्वसन संबंधी समस्या के लिए समय पर चिकित्सा सलाह लें।
प्रश्न 1: एचएमपीवी कैसे फैलता है ?
उत्तरः एचएमपीवी मुख्य रूप से खांसने या छींकने से निकलने वाली ड्रॉपलेट्स, संक्रमित सतहों को छूने के बाद मुंह, नाक, या आंखों को छूने, संक्रमित व्यक्ति के निकट संपर्क में आने से फैलता है।
प्रश्न 2: एचएमपीवी के लिए सबसे अधिक जोखिम में कौन हैं ?
उत्तरः बच्चे विशेष रूप से 5 साल से कम उम्र के, बुजुर्ग जिनकी उम्र 65 वर्ष से अधिक है, कमजोर प्रतिरक्षा प्रणाली वाले व्यक्ति यानी कैंसर, एचआईवी या अन्य गंभीर बीमारियों से ग्रस्त व्यक्ति अधिक प्रभावित है। इसके अलावा पूर्व में श्वसन या हृदय की समस्याएं झेल रहे लोग भी शामिल है।
प्रश्न 3: क्या एचएमपीवी का कोई टीका है ?
उत्तरः वर्तमान में एचएमपीवी के लिए कोई टीका उपलब्ध नहीं है। हालांकि शोधकर्ता इस पर काम कर रहे हैं। संक्रमण से बचाव के लिए व्यक्तिगत स्वच्छता और सावधानियां सबसे प्रभावी उपाय हैं।
प्रश्न 4: एचएमपीवी का इलाज कैसे किया जाता है ?
उत्तरः एचएमपीवी के लिए कोई विशिष्ट एंटी वायरल दवा उपलब्ध नहीं है। उपचार मुख्य रूप से लक्षणों को नियंत्रित करने पर केंद्रित है। बुखार के लिए पैरासिटामोल दी जाती है। तरल पदार्थ की भरपूर मात्रा के अलावा गंभीर मामलों में अस्पताल में ऑक्सीजन सपोर्ट या वेंटिलेटर की आवश्यकता हो सकती है।
प्रश्न 5: क्या एचएमपीवी एक बार होने के बाद दोबारा हो सकता है ?
उत्तरः हां एचएमपीवी से दोबारा संक्रमित होने की संभावना होती है, क्योंकि वायरस के खिलाफ प्रतिरक्षा लंबे समय तक टिकाऊ नहीं रहती। इसलिए सतर्क रहना और सावधानियां बरतना आवश्यक है।

Human metapneumovirus (HMPV) is a type of common respiratory virus that mimics the symptoms of the common cold. It belongs to the Paramyxoviridae family, closely related to the viruses that cause measles and mumps. While most cases infected by the virus are mild, some people are likely to get severely sick, especially the first time they get HMPV infection.
The HMPV infection is more common in winters and early spring but can occur at any time of the year. It affects people of all age groups, although infants and young children, older adults, and people with weakened immune systems are more vulnerable. Untreated cases of HMPV can develop into serious complications, such as pneumonia or bronchitis, therefore if your symptoms last for more than two weeks or become severe, seek medical help immediately.
Whether you’re looking to safeguard your family against the virus or seeking treatment for your child’s existing pediatric human metapneumovirus infection, understanding HMPV is the first step towards effective care.
For HMPV diagnosis, treatment or care, consult Felix Hospital, the best hospital for human metapneumovirus treatment in Noida and Greater Noida.
Human Metapneumovirus is highly contagious and spreads through respiratory droplets, close contact, or contaminated surfaces. Also, once HMPV enters your body, the incubation period lasts between three to six days.
Impact on Adults: Human Metapneumovirus infections in adults can range from mild cold-like symptoms to severe respiratory distress in high-risk groups, such as those with chronic lung diseases and cancer patients.
Impact on Children: Pediatric human metapneumovirus infection is particularly concerning, as it can cause bronchiolitis and pneumonia in infants and toddlers.
Like any virus, human metapneumovirus is contagious, which means it gets transmitted from an infected person. You might get exposed to the virus if you:
Touch surfaces that contain the virus, such as door handles, phones, etc.
Touch your mouth, nose, or eyes after you touch infected surfaces
Come in contact with respiratory droplets from an infected person. It could be through sneezing, spitting, or coughing
Come in direct contact with infected person, such as shaking hands, hugging and touching
Human metapneumovirus is seasonal and is more prevalent during winter or early spring months, same time as flu season.
Infants, young children, and older adults are at greater risk due to weaker immune defenses.
Individuals with pre-existing conditions such as asthma, chronic obstructive pulmonary disease (COPD), or other respiratory conditions are at heightened risk.
Individuals with weakened immune systems, such as those undergoing chemotherapy, are more vulnerable.
The symptoms of HMPV often mimic those of the flu or common cold that usually go away between two to five days. The symptoms can vary in severity depending on the individual’s age, immune status, and overall health.
Cough
Sore throat
Fever
Wheezing
Headache
If left untreated, symptoms can worsen and cause serious health issues in more severe cases, or patients with compromised immune systems. They may experience
Difficulty breathing
Asthma flare-ups
Respiratory infections such as bronchitis or pneumonia
Unless you’re very sick and hospitalized with HMPV, there’s a high chance that you won’t even know that you've been infected with the virus. However, diagnosing HMPV involves a combination of clinical evaluation and diagnostic testing:
Physical Examination: Your doctor will look for symptoms like wheezing, fever, and nasal discharge.
Swab Test: A soft-tipped stick (swab) is used to get a sample from your nose or throat. The sample is sent to the lab for confirmation of the virus.
Blood Tests: Complete blood counts (CBC) and inflammatory markers help evaluate the severity of the infection.
Molecular Tests: Reverse transcription-polymerase chain reaction (RT-PCR) tests detect the presence of HMPV RNA in respiratory samples.
Antigen Detection: Rapid antigen tests help identify the virus, especially in acute cases.
Bronchoscopy/Chest X-rays: Imaging may be required to rule out pneumonia or other complications in the airways of your lungs.
Currently, there’s no treatment for an upper respiratory infection caused by HMPV. Most people can easily manage their symptoms at home and rest until they feel better. The treatment for HMPV primarily focuses on management of symptoms that includes:
Coping with Symptoms: Take over-the-counter medications and cough syrups for fever, cough and pain. Nasal decongestants and saline nasal sprays can be used for congestion in the nose.
Hydration and Rest: Make sure you drink plenty of water and there's adequate fluid intake. Rest is crucial for recovery.
Oxygen Therapy: For severe cases involving respiratory distress, supplemental oxygen may be required.
Hospitalization: Pediatric or elderly patients with complications may need hospitalization.
At Felix Hospitals, the best hospital for human metapneumovirus treatment in Noida, our specialists provide comprehensive care, ensuring patients receive the tailored treatments and care.
You can reduce your risk of getting HMPV by taking these preventive measures:
Washing/Sanitizing your hands often with soap and water or hand sanitizer.
Cover your nose and mouth with your elbow while sneezing or coughing.
Avoid being around or coming in physical contact with an infected person.
Wearing a mask if you’re sick.
Regularly clean and disinfect high-touch surfaces like doorknobs and mobile phones.
Consume a balanced diet, exercise regularly, and avoid smoking to strengthen your immune system.
Don’t share towels, food or eating utensils with others.
Mild cases of human metapneumovirus usually last 3 to 7 days. If you’re very sick, it’ll probably take longer to recover. You might also have lingering symptoms, like a cough, that may take a little longer to go away.
At Felix Hospitals, we have the best doctors for human metapneumovirus (HMPV) treatment in Noida. Our multidisciplinary team combines expertise in pulmonology, internal medicine, pediatrics, and infectious diseases to deliver exceptional care. Leading the way, Dr. Priyadarshi Jitendra Kumar works alongside our highly skilled internal medicine specialists, including Dr. Anshumala Sinha, Dr. Sonakshi Saxena, Dr. Apoorva Shetty, Dr. Neelabh Pratap, Dr. Priyanka Singh, Dr. Ravi Sharma, and Dr. Keshav Kumar Garg.
Whether you need an outpatient consultation or inpatient care, our state-of-the-art facilities and personalized treatment plans ensure a seamless recovery process. At Felix Hospitals, your health is our priority.
Protect yourself and your loved ones from human metapneumovirus. Visit Felix Hospitals, the best hospital for human metapneumovirus treatment, and take proactive steps to safeguard your respiratory health.
Human metapneumovirus is a virus that causes upper and lower respiratory infections. While there’s no cure or vaccine for human metapneumovirus, most cases recover within a few days. However, sometimes infants, older people, and people who have weakened immune systems can develop complications, like pneumonia. Therefore, understanding its symptoms, diagnosis, and treatment options is vital for effective management of HMPV. By taking preventive measures and seeking timely medical care, you can reduce the risk of complications and ensure a faster recovery.
For appointments, contact us at +(91) 9667064100.
At Felix Hospitals, we offer diagnosis and treatments for respiratory infections for patients of all ages.
1- How long does it take to recover from human metapneumovirus?
ANS: It largely depends on the individual’s overall health, age, and immunity. It’s crucial for anyone with existing respiratory symptoms, or compromised immune system to seek medical advice.
2- When should I see my doctor for pediatric human metapneumovirus infection?
ANS: You should seek medical advice if your child’s symptoms don’t start to improve within a few days or if you or your child has a fever lasting longer than three days. If your child has symptoms of a respiratory infection and an underlying condition that puts them at an elevated risk for severe illness, do not delay seeking treatment for pediatric human metapneumovirus infection.
3- Do I need antibiotics for human metapneumovirus?
ANS: No, HMPV is a virus and antibiotics only treat bacteria. However, if your doctor prescribes antibiotics, it would be to treat any secondary infections.
4- What are the complications of human metapneumovirus infections in adults?
ANS: Sometimes HMPV causes complications such as asthma, COPD flare-ups, pneumonia and bronchitis.
5- How is human metapneumovirus transmitted?
ANS: HMPV spreads through direct contact with someone who has it or from touching things contaminated with the virus.

Pulmonary Endarterectomy (PEA) is a complex yet lifesaving surgical procedure for those suffering from chronic thromboembolic pulmonary hypertension (CTEPH). This surgery aims to remove blockages in the pulmonary arteries, improving blood flow and relieving symptoms such as shortness of breath and chest pain. For anyone considering this surgery, it's essential to choose the best hospital for Pulmonary Endarterectomy to ensure optimal outcomes and advanced post-operative care. Felix Hospital provides high-quality care with a team of experienced specialists, including Dr. Priyadarshi Jitendra Kumar, renowned for his expertise in pulmonology.
If you or a loved one is dealing with CTEPH, don’t hesitate to Click Here to reach out to Felix Hospital.
Pulmonary Endarterectomy (PEA) is a highly specialized surgical procedure used to treat CTEPH by removing organized blood clots from the pulmonary arteries. When blood clots from deep veins lodge in the pulmonary arteries, they obstruct blood flow and can lead to increased pressure in the lungs, resulting in CTEPH. PEA surgery removes these obstructions, allowing blood to flow freely, reducing lung pressure, and improving oxygenation.
Surgery is typically required in patients with CTEPH when:
1. Significant Blockage: Persistent blood clots obstruct the pulmonary arteries, causing increased pressure and symptoms.
2. Severe Symptoms: Patients experience severe shortness of breath, fatigue, or chest pain that impacts their quality of life.
3. Ineffectiveness of Medication: For some patients, medications are ineffective in managing CTEPH, making surgery the best option.
4. Risk of Heart Failure: Elevated lung pressure can lead to heart strain or right heart failure if untreated.
PEA is often a last-resort option, usually considered after confirming that other treatments or medications won’t suffice.
CTEPH primarily arises from unresolved pulmonary embolisms (PEs) or blood clots that form in the deep veins, usually in the legs, and travel to the lungs. When these clots do not dissolve, they can permanently lodge in the pulmonary arteries, causing long-term pressure and damage.
Other factors that may contribute to the development of CTEPH include:
Genetic predispositions
Chronic inflammatory or autoimmune conditions
Certain blood disorders
Previous surgeries or trauma
To accurately diagnose CTEPH and determine if PEA surgery is appropriate, a series of tests and imaging studies are performed:
1. Pulmonary Angiography: This imaging test provides detailed visuals of the pulmonary arteries to locate any obstructions.
2. Echocardiography: This test measures pressure within the pulmonary arteries and assesses heart function.
3. Ventilation-Perfusion (V/Q) Scan: A V/Q scan identifies regions in the lungs where blood flow may be restricted.
4. CT Pulmonary Angiography: CT angiography allows doctors to view blood flow within the pulmonary arteries and identify any blood clots.
5. Right Heart Catheterization: This procedure helps measure blood pressure in the lungs to confirm the presence of CTEPH.
The prognosis for patients undergoing PEA surgery is generally favorable, especially when treated at a well-equipped facility with expert surgeons. PEA provides substantial symptom relief, improved quality of life, and increased survival rates, though results can vary based on individual health factors. The cost of a Pulmonary Endarterectomy surgery depends on factors such as hospital facilities, surgeon fees, and post-operative care requirements. Patients are encouraged to discuss the expected costs with their healthcare provider to prepare for both the surgery and the recovery phase.
At Felix Hospital, we’re proud to have Dr. Priyadarshi Jitendra Kumar, one of the best pulmonologists, specializing in pulmonary surgeries and advanced respiratory care. Dr. Kumar’s extensive experience and patient-centered approach make him the ideal choice for anyone considering a PEA.
Pulmonary Endarterectomy is a challenging yet rewarding surgery that offers hope to those struggling with CTEPH. Choosing a hospital with the expertise, resources, and skilled pulmonologists can make a significant difference in your treatment outcome. At Felix Hospital, our team is here to provide comprehensive support through every stage of your journey to better lung health.
Ready to learn more about Pulmonary Endarterectomy and how we can help? Contact Felix Hospital today at +91 9667064100.
1. What is the main goal of Pulmonary Endarterectomy?
ANS: The main goal is to remove blood clots from the pulmonary arteries to restore normal blood flow and relieve symptoms of CTEPH.
2. Who qualifies for Pulmonary Endarterectomy?
ANS: Patients with CTEPH, where medications are ineffective, and the risk of heart failure is present, may be candidates.
3. How long is the recovery period?
ANS: Recovery varies, but most patients can resume normal activities within a few months, with gradual improvement over time.
4. What are the risks associated with PEA?
ANS: While generally safe, risks include bleeding, infection, or recurrence of symptoms, especially in patients with severe pre-existing conditions.
5. How effective is PEA in treating CTEPH?
ANS: PEA is highly effective, providing substantial symptom relief and improving the quality of life for many patients.
6. Is the procedure painful?
ANS: The surgery is performed under anesthesia, so patients do not experience pain during the procedure. Post-operative discomfort is managed with medications.
7. Does insurance cover the cost of Pulmonary Endarterectomy?
ANS: Many insurance plans cover the surgery, but coverage varies. It’s advisable to confirm with your provider.
8. Can lifestyle changes help after surgery?
ANS: Yes, lifestyle changes like regular exercise, a balanced diet, and avoiding smoking can enhance post-surgery recovery and overall health.
9. How do I prepare for PEA surgery?
ANS: Preparation includes medical evaluations, lifestyle adjustments, and following your doctor’s guidance on diet and medications leading up to surgery.

Winter’s arrival brings not only shorter days and colder temperatures but also unique challenges for people with respiratory conditions like asthma and bronchitis. Cold, dry air and sudden temperature shifts can aggravate symptoms, leading to increased coughing, wheezing, and shortness of breath. Understanding why these conditions worsen during winter and how to manage them can be life-changing for asthma and bronchitis patients. Seeking expert guidance and care at the best hospital for respiratory conditions can be instrumental in effectively managing these seasonal challenges.
schedule a consultation with a respiratory specialist today to learn more about managing your condition through the colder months. Call Now at +91 9667064100.
Cold air poses unique challenges for the respiratory system. The lungs and airways function optimally at body temperature, around 37°C (98.6°F). When exposed to cold air, the airways constrict to prevent cold air from entering the lungs, a natural defense that can inadvertently lead to increased respiratory resistance. For individuals with asthma or bronchitis, this reaction can exacerbate inflammation in the airways, leading to the discomfort associated with winter exacerbations.
Dry, Cold Air: Winter air is often dry, which irritates the airways and triggers bronchoconstriction, making it harder for asthma and bronchitis patients to breathe comfortably.
Allergens: Winter often brings an increase in indoor allergens such as dust mites, pet dander, and mold, as people spend more time indoors.
Respiratory Infections: Winter is also flu season, and respiratory infections tend to rise, increasing the risk of complications for people with respiratory conditions.
Asthma is a chronic condition characterized by inflamed and narrow airways. For asthma patients, winter means a higher risk of asthma attacks, which can occur due to cold, dry air, and other seasonal triggers like respiratory infections. During an asthma attack, symptoms like wheezing, coughing, and chest tightness increase, often requiring immediate attention and medication.
Bronchitis can be either acute or chronic. Acute bronchitis usually results from a respiratory infection, while chronic bronchitis, a type of chronic obstructive pulmonary disease (COPD), is often caused by long-term exposure to irritants like cigarette smoke. Winter weather is challenging for bronchitis patients, as cold air triggers the airways to produce more mucus, leading to persistent cough and discomfort.
Airway Constriction: Cold air causes blood vessels in the airways to constrict, which can reduce the amount of oxygen reaching the lungs.
Increased Mucus Production: Cold weather triggers mucus glands, leading to thicker mucus, which clogs airways and makes breathing harder.
Reduced Immunity: Winter can suppress immune function, making it easier to catch infections that further worsen respiratory issues.
More Indoor Exposure: Indoor heating can dry out the air, and an increase in dust, pet dander, and mold can irritate airways.
Avoid going outside during particularly cold or windy days. If you must go out, wear a scarf or mask over your mouth and nose to help warm the air before it enters your lungs.
Using a humidifier at home can add moisture to the dry winter air, making it easier to breathe. Ideal humidity levels are between 30% and 50%, as too much humidity can encourage mold growth and dust mites.
For asthma patients, cold weather exercise can trigger symptoms. Take time to warm up before exercising, and try to exercise indoors when possible.
Cold weather can reduce the sensation of thirst, but staying hydrated is essential to keep mucus thin, which helps prevent airway blockage.
Smoke from fireplaces, candles, and even cooking can irritate the airways. Avoiding these and any strong scents can help reduce symptoms.
Asthma and bronchitis patients should consult their healthcare providers before winter for an updated treatment plan. Common medications include:
Inhaled Corticosteroids: Reduce inflammation and prevent winter flare-ups.
Bronchodilators: Open airways and make breathing easier.
Antibiotics (for bronchitis): Only if bacterial infection is confirmed.
Leukotriene Modifiers: Help control asthma symptoms.
It’s essential to have a quick-relief inhaler on hand for sudden symptoms. Additionally, the Cost of treating asthma and bronchitis can vary depending on the severity of the condition, treatment duration, and location.
Healthy Diet: Eating a balanced diet with plenty of fruits, vegetables, and lean proteins can help boost the immune system.
Regular Exercise: Even in winter, physical activity strengthens the respiratory muscles, although indoor exercises may be better.
Manage Stress: Stress can trigger asthma and bronchitis symptoms. Practice relaxation techniques like deep breathing and meditation.
Get a Flu Shot: Since respiratory infections worsen symptoms, a flu shot can help prevent severe respiratory complications.
Asthma and bronchitis patients must recognize when symptoms require immediate medical attention. Signs include:
Persistent chest pain or pressure
Severe shortness of breath
Bluish lips or face
Confusion or dizziness
With over 20 years of dedicated experience in pulmonary care with the best pulmonologist in Noida, Dr. Priyadarshi Jitender Kumar stands out as a leading expert in diagnosing and treating pulmonary embolism. Known for his thorough approach and personalized care plans, Dr. Kumar has earned a reputation as one of the most trusted specialists in managing this complex condition.
Get Expert Help for Your Winter Respiratory Care. Click here now to book an appointment and breathe easier this winter!
Winter poses unique challenges for asthma and bronchitis patients due to cold air, dry conditions, and increased indoor allergens. However, by taking preventive steps, managing medications, and recognizing early symptoms, patients can navigate the season with better control over their respiratory health. Always consult healthcare providers for personalized advice, and stay prepared to breathe easier through the winter months.
1-How does winter affect asthma and bronchitis?
ANS: Winter's cold, dry air and increased indoor allergens can irritate the airways, leading to increased symptoms like coughing, wheezing, and shortness of breath.
2- Can cold weather make bronchitis worse?
ANS: Yes, cold air can trigger mucus production and airway constriction, worsening symptoms for bronchitis patients.
3- What should I do if my asthma gets worse during winter?
ANS: Consult your doctor for an updated treatment plan, use prescribed inhalers, and take precautions like wearing a scarf over your mouth when outside.
4- Is it safe for asthma patients to exercise outside in winter?
ANS: It can be challenging, as cold air can trigger asthma symptoms. If exercising outside, warm up beforehand, cover your mouth and nose, or consider indoor exercise.
5-Does using a humidifier help with asthma and bronchitis?
ANS: Yes, a humidifier can add moisture to dry winter air, which can ease breathing for asthma and bronchitis patients. Keep humidity levels between 30%-50%.
6- What medications help control winter asthma symptoms?
ANS: Common medications include inhaled corticosteroids, bronchodilators, and leukotriene modifiers, but it’s essential to consult a doctor for the best treatment plan.
7- Should I get a flu shot if I have asthma or bronchitis?
ANS: Yes, a flu shot is recommended as respiratory infections can worsen asthma or bronchitis symptoms during winter.
8-How can I prevent asthma attacks caused by cold air?
ANS: Wear a scarf or mask over your mouth to warm the air before it enters your lungs, avoid strenuous outdoor activity in extreme cold, and stay on top of your medications.
9- Can allergies affect asthma and bronchitis in winter?
ANS: Yes, indoor allergens like dust mites, pet dander, and mold can worsen asthma and bronchitis symptoms as people spend more time indoors in winter.

Sarcoidosis is a complex autoimmune disease that can have a profound effect on multiple organs in the body, particularly the lungs and lymph nodes. The condition occurs when clusters of inflammatory cells, called granulomas, form in various tissues, leading to a range of symptoms and complications. For those seeking effective management and treatment options, it is essential to consult a leading healthcare facility known for its expertise in treating sarcoidosis. Finding the best hospital for sarcoidosis treatment can make a significant difference in achieving optimal health outcomes and improving quality of life.
Take the first step towards a healthier future. Contact us today at +91 9667064100 to schedule a consultation!
Sarcoidosis is an inflammatory disease characterized by the formation of small clusters of inflammatory cells, known as granulomas, in different organs. While the exact cause of sarcoidosis remains unknown, it can affect anyone, although it is more prevalent in adults aged 20 to 40 and tends to affect women more than men. The condition may resolve on its own in some individuals, while others may experience chronic symptoms requiring long-term management.
Sarcoidosis manifests with a diverse array of symptoms that can vary widely depending on the organs affected by the disease. Some of the most common symptoms include:
Fatigue: Many individuals experience persistent tiredness that doesn’t seem to improve with rest, making daily activities challenging.
Shortness of Breath: This symptom can manifest as difficulty breathing, particularly during physical exertion, and may worsen over time.
Cough: Patients may develop a dry cough that can become chronic, contributing to discomfort and hindering daily life.
Skin Rashes: Various skin conditions, including erythema nodosum, can appear, presenting as red, tender lumps or lesions on the skin.
Joint Pain: Swelling, stiffness, and discomfort in the joints are common, potentially leading to reduced mobility and quality of life.
Fever and Night Sweats: Some individuals may experience unexplained fevers and excessive sweating at night, disrupting sleep patterns.
Weight Loss: Unintentional weight loss can occur without any changes in diet or physical activity, signaling potential underlying issues.
The exact etiology of sarcoidosis remains elusive, but several contributing factors have been identified:
Genetic Predisposition: A family history of sarcoidosis may increase the likelihood of developing the condition, suggesting a genetic component.
Environmental Factors: Exposure to certain environmental agents, such as dust, mold, chemicals, or other allergens, may trigger sarcoidosis in susceptible individuals.
Infections: While some infections have been associated with sarcoidosis, their role as definitive causes is still under investigation.
The diagnosis of sarcoidosis typically involves a comprehensive approach, including:
Medical History and Physical Examination: A thorough review of symptoms and medical history, coupled with a physical exam, is the first step.
Imaging Tests: Chest X-rays and CT scans are essential for visualizing potential granulomas in the lungs and assessing lung health.
Biopsy: To confirm the presence of granulomas, a tissue sample from the affected area may be obtained and examined microscopically.
Pulmonary Function Tests: These tests evaluate lung capacity and function, helping to determine the extent of pulmonary involvement.
The treatment of sarcoidosis varies significantly based on the severity of the disease and the organs involved. Common treatment options include:
Medications: Corticosteroids, such as prednisone, are frequently prescribed to reduce inflammation and manage symptoms. In more severe cases, other immunosuppressive drugs, such as methotrexate or azathioprine, may be utilized.
Symptom Management: Depending on the specific symptoms, additional treatments may be recommended to address pain, respiratory issues, or skin conditions, enhancing overall quality of life.
Understanding the cost of sarcoidosis disease treatment in Noida is vital for effective healthcare planning. At Felix Hospitals, we prioritize transparent pricing and strive to provide comprehensive care to ensure patients receive the best treatment possible.
While there is currently no known way to prevent sarcoidosis, adopting a healthy lifestyle may support overall well-being and help manage symptoms. Consider these preventive measures:
Regular Check-ups: Stay proactive about your health with routine medical check-ups, especially if you have a family history of sarcoidosis.
Healthy Lifestyle Choices: A balanced diet rich in fruits, vegetables, and whole grains, along with regular physical activity, can promote lung health and improve immune function. Avoiding smoking is crucial for maintaining respiratory health.
Stress Management: Incorporating stress-reducing practices into your daily routine, such as yoga, meditation, or deep-breathing exercises, can contribute to better overall health and may help mitigate symptoms.
When it comes to sarcoidosis treatment, expertise matters. At Felix Hospitals, we are proud to have the best sarcoidosis doctor in Noida, Dr. Priyadarshi Jitendra Kumar. With extensive experience in managing pulmonary diseases, Dr. Kumar is dedicated to providing compassionate care and effective treatment strategies for patients with sarcoidosis.'
Contact us today to schedule an appointment with Dr. Kumar and take control of your health!
Sarcoidosis is a complex condition that requires careful diagnosis and management. By understanding the causes, symptoms, and treatment options, you can take proactive steps toward better health. If you suspect you may have sarcoidosis or need specialized care, don't hesitate to reach out to the experts at Felix Hospitals.
1-What is sarcoidosis?
ANS: Sarcoidosis is an inflammatory disease characterized by the formation of granulomas in various organs.
2-What causes sarcoidosis?
ANS: The exact cause is unknown, but genetic predisposition, environmental factors, and infections may contribute.
What are the symptoms of sarcoidosis? Symptoms include fatigue, shortness of breath, cough, skin rashes, joint pain, fever, night sweats, and weight loss.
3-How is sarcoidosis diagnosed?
ANS: Diagnosis involves a medical history review, physical examination, imaging tests, biopsies, and pulmonary function tests.
4-What is the treatment for sarcoidosis?
ANS: Treatment often includes corticosteroids and medications to manage symptoms, depending on the severity of the disease.
5-Can sarcoidosis be prevented?
ANS: There is no known prevention method, but maintaining a healthy lifestyle and regular check-ups can support overall health.
6-Who is the best doctor for sarcoidosis treatment in Noida?
ANS: Dr. Priyadarshi Jitendra Kumar at Felix Hospitals is recognized as one of the best sarcoidosis doctors in Noida.
7-What is the cost of sarcoidosis treatment in Noida?
ANS: The cost of treatment varies based on the severity and required medications; it's best to consult Felix Hospitals for accurate pricing.
8-How can I manage sarcoidosis symptoms?
ANS: Follow your doctor’s recommendations, maintain a healthy lifestyle, and engage in stress-reducing activities to help manage symptoms.

Upper respiratory infections (URIs), commonly referred to as colds, are among the most common health concerns affecting individuals of all ages. These infections are usually caused by a variety of viruses and can lead to a range of uncomfortable symptoms, such as nasal congestion, a sore throat, and persistent coughing. Though URIs are typically self-limiting and resolve on their own, understanding the causes, symptoms, and treatment options is essential for effective management. If your symptoms are severe or recurrent, it's crucial to consult the best hospital for respiratory infection treatment in your region for expert care and a comprehensive treatment plan.
If you’re experiencing cold-like symptoms, don’t hesitate to get medical advice. Consult a healthcare provider by calling +91 9667064100.
Upper respiratory infections refer to infections that affect the upper parts of the respiratory system, including the nose, sinuses, throat (pharynx), and larynx (voice box). URIs are predominantly viral and spread easily from person to person. While generally not severe, these infections can be particularly bothersome and may last up to two weeks.
URIs are especially common during cold and flu seasons and are often confused with more serious respiratory conditions. Early identification and management can help prevent complications.
URIs are caused by various types of viruses, which spread through airborne droplets or direct contact with contaminated surfaces. Here are the most common viruses responsible for URIs:
Rhinoviruses: These are the most frequent cause of colds and are responsible for more than half of all cases.
Coronaviruses: These viruses can also cause the common cold, in addition to more severe illnesses like COVID-19.
Adenoviruses: These are associated with respiratory infections, particularly in children.
Respiratory Syncytial Virus (RSV): A virus that causes infections of the lungs and respiratory tract, RSV is especially dangerous for infants and the elderly.
These viruses spread primarily through respiratory droplets released into the air when an infected person sneezes or coughs. You can also contact a URI by touching contaminated surfaces and then touching your face, nose, or mouth.
The symptoms of upper respiratory infections can vary depending on the virus and the individual, but they often include:
Runny or Stuffy Nose: Nasal congestion or a constant runny nose is one of the most common symptoms.
Sore Throat: Inflammation of the throat, often causing discomfort or pain, is typical.
Coughing: A persistent cough can occur as the body's response to clear the airways.
Sneezing: A reflex to help expel the virus from the respiratory tract.
Fatigue: Feeling tired or lethargic is common as the body fights the infection.
Mild Headache: Some people may experience a dull or throbbing headache.
Body Aches: General body discomfort is a frequent symptom of viral infections.
Low-Grade Fever: A mild fever is the body's way of responding to the viral attack.
These symptoms typically appear one to three days after exposure to the virus and last about a week to ten days. However, some people may continue to experience mild symptoms like a cough for several weeks.
Most upper respiratory infections can be diagnosed based on symptoms and a physical examination. A healthcare provider will likely ask about your medical history and the progression of your symptoms. In most cases, no special tests are needed.
However, in certain situations—such as when symptoms are severe or last longer than expected—additional tests may be required to rule out bacterial infections or other underlying conditions, such as:
Throat Swab: A sample from the throat can help detect bacterial infections like strep throat.
Chest X-ray: In rare cases, imaging may be needed to rule out pneumonia or other lung conditions.
Blood Tests: These can help assess your immune response or check for other underlying issues.
Because URIs are viral, antibiotics are ineffective. The main goal of treatment is to relieve symptoms while the body fights off the infection. Here are common treatments:
Rest and Hydration: Resting allows the body to conserve energy to fight the infection. Drinking fluids helps keep you hydrated and supports immune function.
Over-the-counter medications: Decongestants, antihistamines, and pain relievers such as acetaminophen or ibuprofen can alleviate symptoms like nasal congestion, headaches, and body aches.
Steam Inhalation: Inhaling steam from a bowl of hot water can help clear nasal congestion and soothe irritated airways.
Saline Nasal Sprays: These can help clear a stuffy nose and keep the nasal passages moist.
Warm Salt Water Gargle: Gargling with warm salt water can relieve a sore throat and reduce inflammation.
While these measures are often sufficient, some patients may need more advanced treatment depending on the severity of symptoms. It’s important to be aware of the Respiratory infection treatment cost, which may vary depending on the medical facility, diagnostic tests, and the specific treatments required.
Preventing upper respiratory infections involves maintaining good hygiene and supporting your immune system. Consider the following measures:
Frequent Handwashing: Wash your hands thoroughly with soap and water, especially after being in public places or after coughing/sneezing.
Avoid Close Contact: Limit close contact with people who are sick, and avoid sharing personal items like utensils or cups.
Healthy Lifestyle: A balanced diet, regular exercise, and adequate sleep help strengthen your immune system.
Vaccinations: Getting vaccinated against flu viruses can help prevent certain respiratory infections.
Disinfect Surfaces: Regularly clean frequently touched surfaces like doorknobs, phones, and countertops.
If you require specialized care for a respiratory infection, Dr. Priyadarshi Jitendra Kumar, an expert pulmonologist at Felix Hospital, can provide advanced care for respiratory conditions, ensuring personalized treatment and thorough medical attention.
Experiencing cold symptoms or respiratory discomfort? Don’t wait! To seek expert medical care just Click Here.
Upper respiratory infections are common, but understanding the symptoms and treatment options is key to managing them effectively. Whether it's simple home care or consulting a professional, taking the right steps early on can prevent complications. If you or a loved one is suffering from an upper respiratory infection, consult a healthcare provider who specializes in upper Respiratory infection treatment for accurate diagnosis and treatment.
What causes upper respiratory infections?
AND: URIs are primarily caused by viruses such as rhinoviruses, coronaviruses, and adenoviruses.
How can I differentiate between a cold and a more serious illness?
AND: If your symptoms are severe, last longer than 10 days, or worsen over time, seek medical advice.
How long do colds usually last?
AND: Most colds resolve within 7 to 10 days, although a lingering cough can last for a few weeks.
Are antibiotics necessary for colds?
AND: No, antibiotics are ineffective against viral infections such as colds.
How can I prevent catching a cold?
AND: Regular handwashing, avoiding close contact with sick individuals, and maintaining a healthy lifestyle can reduce the risk of infection.
What home remedies can help alleviate cold symptoms?
AND: Drinking plenty of fluids, resting, using saline nasal sprays, and steam inhalation can help relieve symptoms.
When should I seek medical attention for a cold?
AND: If you develop a high fever, difficulty breathing, or severe throat pain, it’s important to consult a healthcare professional.
What is the average cost of respiratory infection treatment?
AND: The Respiratory infection treatment cost varies depending on the healthcare provider and the treatments required, so it's advisable to check with your medical provider for specific costs.
Coughing up blood, or hemoptysis, can be alarming and may indicate a serious underlying medical condition. Early detection and appropriate care are essential, especially when dealing with respiratory issues. For those experiencing such symptoms, seeking care from the best hospital for pulmonology treatment in Noida ensures you receive timely and expert diagnosis and treatment. Understanding the causes, symptoms, and treatment options for hemoptysis is crucial for managing this condition effectively.
If you or a loved one is experiencing hemoptysis, seek medical attention immediately. Click Here to Book Your Appointment.
Hemoptysis refers to coughing up blood from the lungs or respiratory tract. This may range from blood-streaked sputum to larger amounts of blood. While it can be caused by minor conditions such as respiratory infections, it can also indicate more severe issues like lung cancer, tuberculosis, or pulmonary embolism. Understanding the underlying causes is vital to ensure appropriate treatment and prevent complications.
Several conditions can lead to hemoptysis, ranging from mild infections to life-threatening diseases. Common causes include:
1. Respiratory Infections: Bronchitis, pneumonia, and tuberculosis are some infections that can cause irritation and lead to coughing up blood.
2. Chronic Obstructive Pulmonary Disease (COPD): This long-term lung disease can damage blood vessels, leading to hemoptysis.
3. Lung Cancer: One of the more severe causes, hemoptysis can be an early sign of lung cancer.
4. Pulmonary Embolism: A blood clot in the lung can rupture blood vessels, causing blood to be coughed up.
5. Bronchiectasis: A condition where the airways become widened and scarred, leading to frequent infections and hemoptysis.
6. Trauma: Injury to the chest or respiratory system can also result in coughing up blood.
7. Pulmonary Edema: Accumulation of fluid in the lungs, often due to heart failure, can sometimes result in blood-streaked sputum.
8. Medications: Certain blood thinners or anticoagulants can increase the likelihood of hemoptysis.
The primary symptom of hemoptysis is the presence of blood when coughing. However, the amount and appearance of the blood can vary. Accompanying symptoms may include:
Shortness of breath
Chest pain or discomfort
Wheezing
Fever, especially if the cause is an infection
Rapid heart rate
Fatigue
If hemoptysis is accompanied by these signs, especially large amounts of blood, it is a medical emergency that requires immediate attention.
Diagnosing the cause of hemoptysis involves a thorough evaluation, which may include:
1. Medical History and Physical Examination: A detailed review of your medical history and physical exam will help in identifying any underlying conditions.
2. Chest X-ray: To check for infections, tumors, or other abnormalities in the lungs.
3. CT Scan: Provides a more detailed image of the lungs and can help detect blood clots, tumors, or other issues.
4. Bronchoscopy: A procedure where a thin tube with a camera is inserted into the lungs to visually examine the airways.
5. Sputum Tests: Analyzing the sputum (mucus) coughed up can help identify infections like tuberculosis.
6. Blood Tests: To check for infections, bleeding disorders, or other potential issues.
Treatment for hemoptysis depends on the underlying cause and the severity of the condition. Common treatments include:
1. Medications: Antibiotics for infections, bronchodilators for COPD, and other targeted medications depending on the cause.
2. Oxygen Therapy: For patients experiencing difficulty breathing, oxygen may be provided to stabilize their condition.
3. Bronchial Artery Embolization: This is a minimally invasive procedure to stop severe bleeding in the lungs.
4. Surgery: In cases of severe trauma, tumors, or life-threatening conditions, surgery may be required to stop bleeding or remove a tumor.
5. Hospitalization: Patients with significant bleeding may need to be hospitalized for close monitoring and treatment.
Understanding the Pulmonary Treatment cost associated with these interventions is important. Costs can vary based on the severity of the condition, the treatments required, and the hospital providing the care.
Preventing hemoptysis involves addressing the root causes and maintaining good lung health. Some preventive measures include:
1. Quit Smoking: Smoking is a significant risk factor for lung diseases, including cancer, COPD, and bronchitis, which can cause hemoptysis.
2. Vaccinations: Keeping up with vaccines like the flu and pneumonia vaccines can help prevent respiratory infections that lead to hemoptysis.
3. Manage Chronic Conditions: Proper management of chronic conditions like COPD, heart failure, and bronchiectasis can reduce the likelihood of hemoptysis.
4. Use Protective Gear: For those working in environments with harmful chemicals or pollutants, wearing protective equipment can help prevent lung damage.
The prognosis for hemoptysis depends on the underlying cause. For example:
Infections are often treatable with medication, and the prognosis is generally good.
Hemoptysis caused by lung cancer or pulmonary embolism requires more intensive treatment, and the outlook varies depending on how early the condition is diagnosed and treated.
Early detection and treatment are key to improving outcomes, which is why it’s essential to consult a pulmonologist as soon as symptoms occur.
Choosing the best pulmonologist in Noida is vital for effectively diagnosing and managing hemoptysis. At Felix Hospital, Dr. Priyadarshi Jitendra Kumar are renowned specialist with years of experience in treating respiratory conditions, including hemoptysis. With state-of-the-art facilities and personalized care, our team is dedicated to providing the best outcomes for our patients. Whether you're facing a mild issue or a serious concern, our expert pulmonologists are here to help.
Contact Felix Hospital today at +91 9667064100 to schedule a consultation with our top pulmonologists and receive expert care tailored to your needs.
Hemoptysis, or coughing up blood, is a serious symptom that should not be ignored. Whether it's caused by a simple infection or a more severe condition like lung cancer, early diagnosis and appropriate treatment are critical for a good outcome. If you're experiencing hemoptysis or other respiratory symptoms, don’t hesitate to consult a specialist at the Best pulmonology hospital in Noida. With the right care, you can manage the condition effectively and improve your quality of life.
1. What is hemoptysis?
ANS: Hemoptysis refers to coughing up blood from the lungs or respiratory tract, which may indicate an underlying medical condition.
2. Is hemoptysis always a sign of a serious condition?
ANS: Not necessarily. It can result from infections or minor issues, but it can also indicate severe conditions like lung cancer or pulmonary embolism. It’s essential to seek medical advice.
3. When should I see a doctor for hemoptysis?
ANS: You should see a doctor if you cough up blood, especially if it's accompanied by other symptoms like shortness of breath, chest pain, or a large amount of blood.
4. How is hemoptysis diagnosed?
ANS: Diagnosis typically involves medical history, a physical exam, chest X-rays, CT scans, bronchoscopy, and sputum or blood tests.
5. What are the most common causes of hemoptysis?
ANS: Respiratory infections, chronic obstructive pulmonary disease (COPD), lung cancer, pulmonary embolism, and bronchiectasis are among the most common causes.
6. Can hemoptysis be treated at home?
ANS: Minor cases caused by infections may improve with rest and prescribed medications, but more severe cases require medical intervention.
7. How can I prevent hemoptysis?
ANS: Preventive measures include quitting smoking, managing chronic conditions, staying vaccinated, and reducing exposure to lung irritants.
When dealing with pulmonary edema management the selection of the healthcare provider proves to be essential in achieving effective treatment and successful recovery outcomes. Felix Hospital, a Pulmonary edema Hospital in Noida, prioritizes providing care that caters to the individual requirements of patients grappling with this health condition. Through our state-of-the-art amenities medical staff, and customized treatment strategies we strive to deliver exceptional care and assistance to individuals impacted by pulmonary edema.
Don't delay in booking your consultation today to receive the attention you require! Reach out to Felix Hospital immediately at +91 9667064100.
Experiencing pulmonary edema involves the build-up of fluid in the lungs that hinders breathing and oxygen exchange functions in the body. This condition may arise from health concerns such, as heart ailments, kidney disorders, or pneumonia. It is crucial to diagnose and treat pulmonary edema to prevent severe complications from occurring.
The symptoms of pulmonary edema can range from mild to severe and may include:
Struggling to catch my breath or feeling like I can't breathe properly.
Superficial breaths.
Experiencing wheezing or coughing up frothy pink mucus.
The feeling of puffiness, in the legs or feet
Feeling lacking energy.
Heartbeats that are fast or irregular
If you or a loved one experiences any of these symptoms, it is important to seek medical attention promptly.
Detecting pulmonary edema requires both assessment and specific tests at Felix Hospital where our method involves the following:
Medical History and Physical Examination: Medical background and physical assessment are carefully examined by our experts before further evaluation is conducted.
Imaging Tests: We utilize chest X-rays. Ct scans to observe the buildup of fluid in the lungs.
Echocardiogram: An echocardiogram is performed to evaluate the heart's functionality and detect any heart-related problems that may be causing edema.
Blood Tests: We perform blood tests to assess the functioning of the kidneys and heart health markers well as other significant measures.
At Felix Hospital we offer a range of Acute pulmonary edema treatment choices to help patients deal with pulmonary edema:
Medications: Our experts recommend medications to decrease retention, in the body's tissues and enhance heart performance while tackling the root issues at hand.
Oxygen Therapy: We provide oxygen therapy to boost oxygen levels and alleviate breathing difficulties.
Lifestyle and Dietary Guidance: Our team offers advice, on adjusting your lifestyle and diet to deal with symptoms effectively and reduce the chances of them coming back.
Emergency Care: In cases of urgency or critical conditions, we provide assistance and immediate medical attention to stabilize patients and manage sudden symptoms effectively.
Felix Hospital is known for being a top-notch option, for treating edema because of its exceptional quality of care:
Expert Medical Team: Our team of experts specializing in pulmonary care boasts years of experience and a steadfast commitment, to delivering top-notch healthcare services.
State-of-the-Art Facilities: Cutting-edge Infrastructure Utilized We employ advanced technology to ensure precise diagnosis and successful therapy.
Personalized Care: We customize treatment plans to suit the needs of every patient.
Compassionate Support: Our team provides assistance and understanding throughout treatment.
Discover how Felix Hospital can provide comprehensive care for pulmonary edema and other respiratory conditions.
Visit our website or reach out to our patient services team at +91 9667064100.
Dr. Priyadarshi Jitendra Kumar is a distinguished pulmonologist at Felix Hospital, renowned as the top pulmonary edema treatment doctor with over 20 years of experience in managing respiratory conditions, including pulmonary edema. His extensive expertise and compassionate approach make him a leading choice for patients seeking the highest standard of care.
1. What is pulmonary edema?
Pulmonary edema is a medical condition characterized by the accumulation of fluid in the lungs, which interferes with normal breathing and oxygen exchange. It can result from various underlying conditions, including heart failure, kidney disease, and pneumonia.
2. What are the common symptoms of pulmonary edema?
Common symptoms include shortness of breath, rapid or shallow breathing, coughing up frothy or pink mucus, swelling in the legs or ankles, fatigue, and a rapid or irregular heartbeat. If you or someone you know is experiencing these symptoms, seek medical attention immediately.
3. What causes pulmonary edema?
Pulmonary edema can be caused by several factors, including congestive heart failure, kidney dysfunction, pneumonia, exposure to toxins, and certain medications. Identifying the underlying cause is crucial for effective treatment.
4. What treatment options are available for pulmonary edema at Felix Hospital?
Treatment options at Felix Hospital include medications to reduce fluid buildup and improve heart function, oxygen therapy to alleviate breathing difficulties, lifestyle and dietary guidance, and emergency care for severe cases. Our approach is tailored to each patient’s specific needs.
5. How can lifestyle changes help manage pulmonary edema?
Lifestyle changes such as reducing salt intake, managing fluid consumption, engaging in regular physical activity, and avoiding alcohol and smoking can significantly help in managing pulmonary edema and improving overall health.
6. Is pulmonary edema a life-threatening condition?
Yes, pulmonary edema can be life-threatening if not treated promptly. It can lead to severe respiratory issues and complications if left unmanaged. Early diagnosis and treatment are essential for preventing serious outcomes.
7. How can I make an appointment with Dr. Priyadarshi Jitendra Kumar?
To schedule an appointment with Dr. Priyadarshi Jitendra Kumar, please contact Felix Hospital at +91 9667064100. Our team will assist you in arranging a consultation and discussing your treatment options.

Chronic Obstructive Pulmonary Disease (COPD) can make everyday tasks challenging, especially when it comes to maintaining a healthy diet. Proper nutrition plays a crucial role in managing COPD symptoms, improving overall health, and enhancing quality of life. A well-balanced diet can help strengthen your immune system, maintain healthy lung function, and manage weight effectively. In this blog, we'll explore eight COPD-friendly foods that can support your respiratory health and offer practical tips for incorporating them into your daily meals.
For expert care and guidance, the Best Pulmonary Hospital in Noida offers comprehensive treatment options tailored to your needs. Let's delve into these beneficial foods that can make a positive impact on your COPD management.
Ready to take charge of your COPD management? Discover how a tailored diet plan can make a difference. Contact us today +91 9667064100 to learn more about nutrition for COPD!
8 Foods to Eat When You Have COPD and Why They Are Beneficial
1. Leafy Greens
Why: Spinach, kale and collard green are examples of green leafy vegetables rich in antioxidants and vitamins such as vitamins A, C and K which play a vital role in combating inflammation and oxidative stress thus receiving criticism for worsened symptoms of this condition. Also, thin and delicate constituents such as fresh and green leaves are low in energy requirements hence preventing or reducing the chances of contracting these diseases through excessive calories intake.

For expert care and advice, consider visiting the Best COPD Hospital in Noida, where specialized treatment plans are tailored to help you manage this condition effectively.
2. Fatty Fish
Why: This is particularly true for Omega-3 fatty acids found in such fish as salmon, mackerel and sardines have high inflammatory value. Omega-3s can also be useful in lowering lung inflammation, which is helpful to COPD patients since they are at a higher risk for heart disease too.

3. Berries
Why: Other fruits such as blueberries, strawberries and raspberries are rich in antioxidant vitamin C, which help fight free radicals and support the immune system in case of this condition and promote good lung health.

4. Nuts and Seeds
Why: Almonds and walnuts; chia and flax seeds are examples of foods rich in healthy fats, protein, and fiber in the form of nuts and seeds respectively. These nutrients are anti-inflammatory, contribute toward protection of muscles and provide lasting energy, a benefit for the COPD patient often suffering from fatigue and muscle wasting.

If you're exploring options for managing this condition, understanding the Chronic Obstructive Pulmonary Disease Treatments Cost can help you plan effectively. Proper diet, alongside the right medical care, can make a significant difference in managing these symptoms.
5. Whole Grains
Why: Brown rice, quinoa and products made from whole wheat contain fiber and other nutrients, for instance B vitamins. Fiber is good for the digestive system and weight loss and therefore the management of COPD while B vitamins which assist in the formation of red blood cells needed for oxygenated blood are necessary for energy and lung function.

6. Lean Proteins
Why: Non fatty sources of protein include chicken, turkey, and tofu which are used to cater for amino acid requirements in muscles. This condition patients also need to preserve muscle mass; this is because muscle weakness has been found to limit the functional capacity of such patients and their respiratory effectiveness.

7. Sweet Potatoes
Why: Sweet potatoes are rich in Vitamin A and Vitamin C: which are very important to boost the immune system and reduce inflammation. These nutrients are important for the health of the lungs and for increasing the body's defenses and fighting off diseases and the effects of COPD.

For expert guidance and care, consider consulting the Best Pulmonologist in Noida to develop a comprehensive plan for managing this effectively.
8. Garlic
Why: Garlic also has allicin, which helps in reducing inflammation as well as in building the immune system. Eating garlic is beneficial for the reduction of inflammation, and boosting the immunity which are critical when one has COPD and wants to maintain good respiratory health.

A COPD friendly diet is important for several reasons as discussed before. It can assist in relieving symptoms, controlling life threats and managing overweight. This condition can be managed by following a proper diet plan that has a positive impact on the lung function, on inflammation and immunity to depress the difficulties that are faced by the patients. Further, a well balanced diet is also important for preventing malnutrition and loss of muscles which are concerns amongst COPD patients.
For personalized care, it's important to consult the Best Chronic Obstructive Pulmonary Disease Doctors who can guide you in creating a diet plan that supports your overall health and well-being.
Dt. Pooja Yadav
Dt. The current position holder is Pooja Yadav who holds B. Sc and M. Sc in Nutrition and still 8 years experienced Senior Dietitian at the Felix Hospital. Still, she is famous for creating a special pregnancy diet that does not harm the mother and her unborn child.
Dt. Nida Zafar
Dt. Nida Zafar has a degree of B. Sc and M. Sc in Nutrition she is a very hardworking dietician for 4 years she is specialized in pregnancy diet consultation. She offers tailor made diets which are required to be consumed by pregnant women depending on their health conditions.
Take the first step towards a healthier lifestyle with COPD. Schedule a consultation+91 9667064100 with our dieticians at Felix Hospital to get your customized diet plan today!
COPD is a chronic health condition and its management involves adopting complex measures and one of them is diet . By applying the below-mentioned COPD friendly foods into your diet, it will be helpful to strengthen your respiratory muscles and minimize inflammation thus improving your quality of life.
1. What is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a group of lung conditions that cause breathing difficulties and affect lung function over time.
2. How can diet impact COPD?
A balanced diet can reduce inflammation, improve lung function, and maintain a ji healthy weight, which are crucial for managing COPD.
3. Are there any foods to avoid with COPD?
Yes, it’s advisable to avoid foods high in sodium, saturated fats, and refined sugars, as they can exacerbate symptoms and lead to weight gain.
4. Can I eat dairy products if I have COPD?
Dairy products can sometimes increase mucus production. It’s best to monitor how they affect you personally and adjust your diet accordingly.
5. How important is hydration for COPD patients?
Staying hydrated is essential as it helps keep mucus thin and easier to expel, improving breathing comfort.
6. Can supplements help with COPD?
Supplements may be beneficial, but it’s important to consult with a healthcare provider before starting any new supplements to ensure they are appropriate for your condition.
7. Is it necessary to follow a special diet plan for COPD?
A tailored diet plan can be very helpful in managing symptoms and improving quality of life, and it’s often recommended by healthcare professionals.
8. How can I manage weight with COPD?
Focus on nutrient-dense, low-calorie foods and maintain a balanced diet. Consult with a dietician for a personalized plan.
9. Are there specific recipes that are good for COPD?
Yes, recipes that incorporate the recommended foods like leafy greens, fatty fish, and whole grains can be beneficial. Consulting with a dietician can provide you with recipes suited to your needs.
10. How can I get support for managing my COPD diet?
Seeking advice from a dietician, such as those at Felix Hospital, can provide you with personalized support and help you create an effective diet plan tailored to your needs.
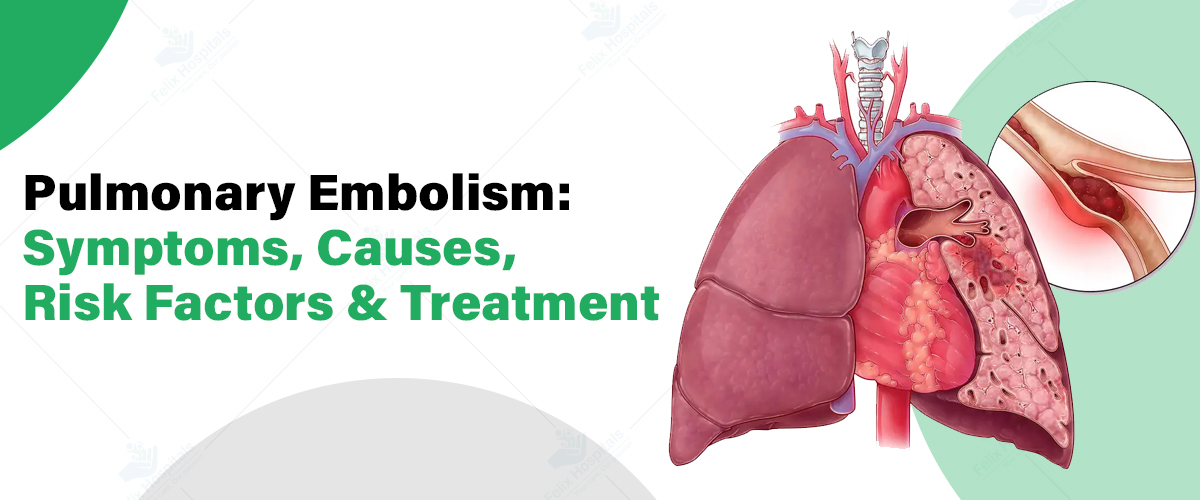
Pulmonary embolism (PE) is a critical condition that arises when a blood clot blocks one or more arteries in the lungs, leading to potentially severe and life-threatening complications. At the forefront of diagnosing and managing this condition is the Best Pulmonology Hospital in Noida, which specializes in comprehensive care for respiratory and vascular issues. Understanding the symptoms, causes, risk factors, and treatment options for pulmonary embolism is essential for timely intervention and effective management. This detailed guide provides crucial insights into how PE develops, how it is diagnosed, and the best practices for treatment and prevention.
Protect Your Lungs: Schedule a Pulmonary Embolism Screening Today! Call Now - +91 9667064100.
Pulmonary embolism (PE) is a serious medical condition that occurs when a blood clot blocks one or more arteries in the lungs. This obstruction impedes blood flow and can lead to severe complications or even be life-threatening. Understanding the symptoms, causes, risk factors, and treatment options for pulmonary embolism is crucial for timely diagnosis and effective management.
The symptoms of pulmonary embolism can vary widely depending on the size of the clot and the extent of the blockage. Common symptoms include:
Pulmonary embolism is primarily caused by blood clots that travel from other parts of the body to the lungs. These clots usually originate in the deep veins of the legs (deep vein thrombosis). Common causes of these clots include:
Diagnosing pulmonary embolism involves a combination of clinical assessment, imaging tests, and laboratory tests:
Treatment for pulmonary embolism aims to dissolve the clot, prevent new clots, and manage symptoms. Treatment options include:
Several factors can increase an individual's risk of developing pulmonary embolism. These include:
Preventive measures are crucial for individuals at risk of pulmonary embolism. These include:
Dr. Priyadarshi Jitendra Kumar is a distinguished pulmonologist with over 20 years of experience in General Practice. He specializes in the comprehensive management of conditions such as diabetes, thyroid disorders, hypertension, infectious diseases, and critical care. His expertise also extends to treating sleep disorders and performing advanced interventional pulmonology procedures.
Pulmonary embolism is a potentially life-threatening condition that requires prompt diagnosis and treatment. Recognizing the symptoms, understanding the causes and risk factors, and seeking timely medical intervention are crucial for managing and preventing PE. For more information or to discuss your concerns with the best pulmonologist in Noida, please contact us today.
1-Why Do You Get Pulmonary Embolism?
Pulmonary embolism occurs when a blood clot blocks one or more arteries in the lungs, obstructing blood flow. The most common cause is a blood clot that originates in the deep veins of the legs, known as deep vein thrombosis (DVT), and travels to the lungs. Other causes include:
2-Can Pulmonary Embolism Be Cured?
Yes, pulmonary embolism can be treated effectively. The treatment aims to dissolve the clot, prevent new clots from forming, and manage symptoms. While there is no cure in the traditional sense, effective management can resolve the clot and reduce complications. Treatments include:
3-Who Is at Risk for a Pulmonary Embolism?
Individuals at higher risk for pulmonary embolism include:
4-What Is the Immediate Treatment for Pulmonary Embolism?
Immediate treatment for pulmonary embolism involves:
5-What Are Pulmonary Embolism Warning Signs?
Common warning signs of pulmonary embolism include:
6-Can a Pulmonary Embolism Be Treated at Home?
Pulmonary embolism generally requires medical intervention and cannot be effectively treated at home. Immediate medical care is essential to manage the condition and prevent complications. Home care might include following medical advice and taking prescribed medications, but the initial treatment and monitoring should be done in a healthcare facility.
7-What Is the Best Treatment for Pulmonary Embolism?
The best treatment for pulmonary embolism depends on the severity and individual patient factors. Standard treatments include:
Early diagnosis and treatment are crucial for effective management and improved outcomes in pulmonary embolism.