
Subscribe to our
Living with Chronic Obstructive Pulmonary Disease (COPD) presents numerous challenges, but with proper management and lifestyle adjustments, individuals can significantly improve their quality of life. One often overlooked aspect of COPD management is nutrition. A well-balanced diet tailored to the specific needs of COPD patients can play a crucial role in managing symptoms, boosting energy levels, and supporting overall health.
In this blog, we'll explore five essential diet tips for people with COPD. These recommendations are designed by the best pulmonary doctor for COPD to help you breathe easier, maintain a healthy weight, and strengthen your body's defenses against respiratory infections.
Looking for effective COPD management? Contact us at +91 9667064100 and take the first step towards better breathing today!
1. Prioritize Protein for Muscle Strength and Repair
For individuals with COPD, maintaining muscle mass is crucial. The respiratory muscles, which are responsible for breathing, can become weakened due to the extra effort required to breathe with compromised lungs. Additionally, many COPD patients experience unintended weight loss and muscle wasting, a condition known as Pulmonary cachexia.
To combat these issues, it's essential to incorporate adequate protein into your diet. Protein is the building block of muscles and plays a vital role in tissue repair and immune function. Aim to include a source of lean protein in every meal.
Good protein sources include:
For those who struggle to eat large meals due to shortness of breath, try incorporating protein-rich snacks throughout the day. Greek yogurt with berries, a handful of almonds, or a hard-boiled egg can provide a quick protein boost without overwhelming your system.
It's important to note that while protein is crucial, excessive protein intake can increase carbon dioxide production, potentially making breathing more difficult. Consult with a registered dietitian to determine the right amount of protein for your individual needs.
2. Balance Carbohydrates for Energy Management
Carbohydrates are the body's primary source of energy, but for chronic obstructive pulmonary disease (COPD) patients, managing carbohydrate intake requires a delicate balance. Consuming too many carbohydrates, especially simple sugars, can lead to increased carbon dioxide production during metabolism. This can potentially worsen breathlessness in some individuals with COPD.
However, it's important not to eliminate carbohydrates entirely, as they are essential for energy production. The key is to focus on complex carbohydrates and practice portion control.
Tips for managing carbohydrate intake:
Choose whole grains over refined grains (e.g., brown rice instead of white rice, whole wheat bread instead of white bread)
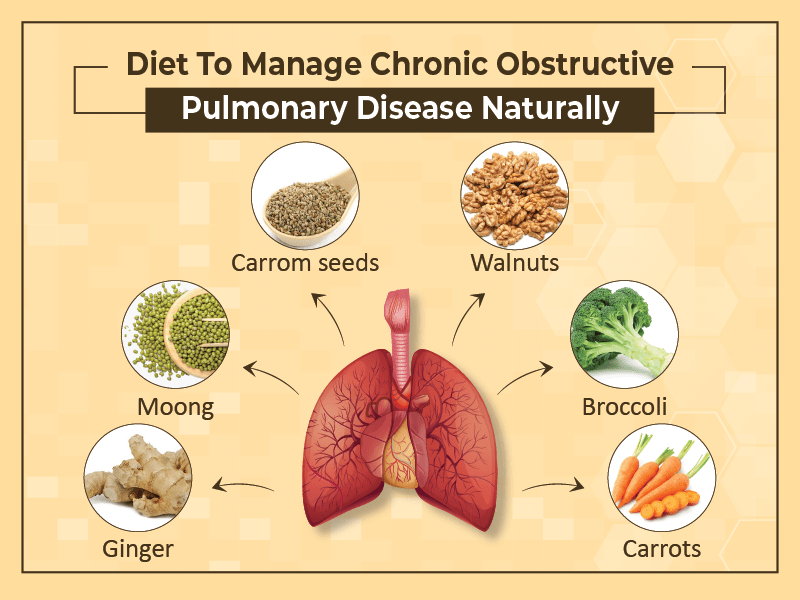
3. Embrace Healthy Fats for Inflammation Reduction
Inflammation plays a significant role in chronic obstructive pulmonary disease (COPD) progression and symptom severity. While medication is often necessary to manage inflammation, dietary choices can also have an impact. Incorporating healthy fats, particularly omega-3 fatty acids, into your diet may help reduce inflammation and support overall lung health.

Beneficial sources of healthy fats include:
Omega-3 fatty acids have been shown to have anti-inflammatory properties. Some studies suggest that regular consumption of omega-3s may help improve lung function and reduce the risk of COPD exacerbations.
While incorporating healthy fats is important, it's crucial to maintain a balance. Fats are calorie-dense, so be mindful of portion sizes, especially if weight management is a concern. Additionally, some COPD patients find that high-fat meals can cause discomfort and make breathing more difficult. If you experience this, try spreading your fat intake throughout the day in smaller portions.
4. Stay Hydrated for Optimal Mucus Management
Proper hydration is crucial for everyone, but it's particularly important for individuals with COPD. Adequate fluid intake helps keep mucus thin and easier to expel, which is essential for maintaining clear airways and preventing infections.
Water is always the best choice for hydration, but other beverages can contribute to your daily fluid intake as well.
Hydration tips for COPD patients:
5. Focus on Nutrient-Dense Foods for Overall Health
COPD can increase the body's energy requirements, making it crucial to maximize the nutritional value of every meal. Focusing on nutrient-dense foods ensures that you're getting the most benefit from the calories you consume.
Nutrient-dense foods are rich in vitamins, minerals, and other beneficial compounds while being relatively low in calories. These foods can help support your immune system, promote healing, and provide the energy needed to manage COPD symptoms.

Some nutrient-dense foods to incorporate into your diet include:
Certain nutrients are particularly important for COPD patients:
Vitamin D: Many COPD patients have low vitamin D levels, which can impact lung function and increase the risk of exacerbations. Good sources include fatty fish, egg yolks, and fortified dairy products. Sun exposure also helps the body produce vitamin D.
Vitamin C: This antioxidant vitamin supports immune function and may help protect lung tissue from damage. Citrus fruits, strawberries, bell peppers, and broccoli are excellent sources.
Vitamin E: Another antioxidant that may help protect lung tissue. Found in nuts, seeds, and vegetable oils.
Magnesium: This mineral supports muscle and nerve function, including the muscles involved in breathing. Good sources include spinach, nuts, seeds, and whole grains.
While a balanced diet should provide most of the nutrients you need, some COPD patients may benefit from supplements. Always consult with your healthcare provider, ideally at the best pulmonary disease hospital, before starting any new supplement regimen, as some supplements can interact with medications or have unexpected effects on COPD symptoms.
Dr. Priyadarshi Jitendra Kumar
Dr. Priyadarshi Jitendra Kumar, MBBS, DNB, FSM, FCCP, brings over 20 years of specialized experience in treating Chronic Obstructive Pulmonary Disease (COPD). Renowned for his expertise in respiratory and sleep medicine, he excels in advanced diagnostic and therapeutic procedures, including flexible bronchoscopy and EBUS. His comprehensive approach and deep knowledge ensure effective management of COPD, tailored to each patient’s needs.
Dt. Pooja Yadav
Dt. Pooja Yadav, B.Sc, M.Sc-Nutrition, is a seasoned dietitian with over 8 years of experience in crafting effective diet plans for managing Chronic Obstructive Pulmonary Disease (COPD). As a Senior Dietitian at Felix Hospital, she specializes in creating personalized nutrition strategies that support respiratory health and improve overall well-being. Her expertise in dietetics ensures that each patient receives tailored dietary interventions to manage COPD effectively and enhance their quality of life.
Dt. Nida Zafar
Dt. Nida Zafar, B.Sc, M.Sc-Nutrition, is a dedicated dietician with 4 years of experience specializing in COPD diet management. She excels in providing personalized dietary counseling for both outpatient and inpatient settings, ensuring tailored nutrition plans that support effective COPD management. Her commitment to staying updated with the latest advancements and her focus on delivering exceptional patient outcomes make her a trusted expert in optimizing respiratory health through diet.
Proper nutrition is a powerful tool in managing COPD and improving overall quality of life. By prioritizing protein, balancing carbohydrates, embracing healthy fats, staying hydrated, and focusing on nutrient-dense foods, individuals with COPD can support their lung health and overall well-being. For optimal results, consider discussing your dietary needs with your healthcare team to complement your chronic obstructive pulmonary disease treatment.
Remember that everyone's nutritional needs are unique, and what works for one person may not be ideal for another. It's essential to work closely with your healthcare team, including a registered dietitian if possible, to develop a nutrition plan tailored to your specific needs and circumstances.
Have further queries about COPD care? Call us at +91 9667064100 or simply click here for expert answers and personalized assistance!
Sure, here are the rephrased questions along with brief answers:
1. What are the different stages of COPD?
COPD is classified into four stages: Stage 1 (mild), Stage 2 (moderate), Stage 3 (severe), and Stage 4 (very severe). Each stage reflects the progression of the disease and its impact on lung function and overall health.
2. What is the primary cause of COPD?
The main cause of COPD is long-term exposure to harmful substances, particularly cigarette smoke. Other factors include prolonged exposure to air pollutants, dust, and fumes.
3. Can COPD be cured?
COPD cannot be cured, but it can be managed effectively. Treatments focus on relieving symptoms, improving quality of life, and slowing disease progression through medications, lifestyle changes, and therapies.
4. What is the most effective treatment for COPD?
The most effective treatment for COPD usually involves a combination of medications (such as bronchodilators and steroids), lifestyle changes (like quitting smoking), and pulmonary rehabilitation to improve lung function and manage symptoms.
5. Is COPD a serious condition?
Yes, COPD is a serious condition. It progressively worsens over time and can significantly impact a person's quality of life, leading to severe breathing difficulties and complications if not properly managed.
6. What does the 6-minute walk test involve for COPD patients?
The 6-minute walk test measures how far a patient can walk in six minutes. It helps assess their exercise tolerance, lung function, and overall health, providing valuable information for managing COPD.
7. Which type of doctor can diagnose COPD?
A pulmonologist, a specialist in respiratory conditions, is typically the doctor who diagnoses COPD. However, general practitioners and internists can also diagnose and manage the disease.
8. How can a doctor determine if you have COPD?
A doctor can diagnose COPD through a combination of medical history, physical examination, and diagnostic tests like spirometry, which measures lung function, and imaging studies such as chest X-rays or CT scans.