
Subscribe to our

Enlarged tonsils and adenoids are often perceived as conditions primarily affecting children, yet they can persist or even develop in adults, leading to a range of health complications. While these issues are typically recognized in younger populations, adult cases are gaining increasing attention in medical circles. This blog aims to provide a comprehensive overview of enlarged tonsils and adenoids in adults, including their causes, symptoms, diagnosis, treatment options, and potential complications. If you are seeking the best ENT surgeon in Noida, understanding these conditions will help you make informed decisions about your health and treatment options.
Schedule a consultation with our experienced healthcare professionals today to receive a personalized treatment plan by Calling +91 9667064100.
The tonsils and adenoids are part of the body's lymphatic system, playing crucial roles in the immune response.
Tonsils: These are two oval-shaped masses of lymphoid tissue located at the back of the throat, one on each side. They help trap pathogens that enter the body through the mouth and nose, producing antibodies to fight infections.
Adenoids: Also known as pharyngeal tonsils, these are located higher up in the throat, behind the nose. Like the tonsils, adenoids help in fighting infections, especially during childhood.
Both structures can become enlarged due to repeated infections, allergies, or other factors.
While enlargement of these tissues is common in children, adults can also experience this condition, often resulting from chronic inflammation or infection. In adults, enlarged tonsils and adenoids can lead to various health issues, including sleep apnea, difficulty swallowing, and recurrent infections.
The enlargement of tonsils and adenoids in adults can result from several factors, including:
Chronic Infections: Repeated infections, such as tonsillitis or adenoiditis, can lead to the enlargement of these tissues. Bacterial or viral infections cause inflammation and swelling.
Allergies: Allergic reactions can contribute to chronic inflammation of the tonsils and adenoids, leading to their enlargement.
Environmental Irritants: Exposure to pollutants, cigarette smoke, or other irritants can cause inflammation and enlargement of these tissues.
Obstructive Sleep Apnea (OSA): In some cases, enlarged tonsils and adenoids can contribute to OSA, a condition characterized by repeated interruptions in breathing during sleep.
Genetic Factors: Some individuals may have a genetic predisposition to enlarged tonsils and adenoids, leading to a higher likelihood of experiencing this condition.
Adults with enlarged tonsils and adenoids may experience a variety of symptoms, which can vary in severity. Common symptoms include:
Difficulty Swallowing: Enlarged tonsils can obstruct the throat, making swallowing painful or difficult.
Persistent Sore Throat: Chronic inflammation can lead to ongoing discomfort in the throat.
Snoring: Enlarged tonsils and adenoids can cause airway obstruction, leading to snoring during sleep.
Sleep Disturbances: Conditions such as obstructive sleep apnea may develop, causing fatigue and excessive daytime sleepiness.
Ear Infections: Blocked Eustachian tubes, which connect the middle ear to the throat, can lead to recurrent ear infections.
Mouth Breathing: Chronic obstruction can force individuals to breathe through their mouths, leading to dry mouth and bad breath.
Swollen Lymph Nodes: Inflammation can cause nearby lymph nodes to swell, particularly in the neck region.
A thorough evaluation by a healthcare professional is essential for diagnosing enlarged tonsils and adenoids. The diagnostic process typically involves:
Medical History Review: The doctor will ask about the patient's symptoms, medical history, and any previous occurrences of infections or allergies.
Physical Examination: A thorough examination of the throat, neck, and ears will be performed to assess the size of the tonsils and adenoids and any signs of infection.
Imaging Tests: In some cases, imaging tests such as X-rays, CT scans, or MRIs may be used to visualize the adenoids and assess their size and position.
Sleep Study: If obstructive sleep apnea is suspected, a sleep study may be conducted to monitor the patient's breathing patterns during sleep.
Treatment for enlarged tonsils and adenoids in adults depends on the severity of the symptoms and the underlying causes. Options include:
For mild cases, conservative management may be sufficient:
Observation: If the symptoms are not severe, doctors may recommend monitoring the condition without immediate intervention.
Home Remedies: Gargling with salt water, staying hydrated, and using humidifiers can help soothe throat irritation.
Over-the-counter Medications: Pain relievers such as acetaminophen or ibuprofen can alleviate discomfort.
If inflammation or infection is present, the following medications may be prescribed:
Antibiotics: If a bacterial infection is diagnosed, antibiotics may be necessary to treat the underlying infection.
Corticosteroids: These medications can help reduce inflammation and swelling in the tonsils and adenoids.
Antihistamines: For allergic reactions, antihistamines can help reduce symptoms and inflammation.
In cases where symptoms are severe or persistent, surgical intervention may be necessary:
Tonsillectomy: This is the surgical removal of the tonsils, commonly performed when chronic infections, sleep apnea, or swallowing difficulties are present.
Adenoidectomy: The surgical removal of the adenoids may be recommended in cases of chronic adenoiditis or obstructive sleep apnea.
Uvulopalatopharyngoplasty (UPPP): In cases of obstructive sleep apnea, this surgery can help remove excess tissue from the throat to widen the airway.
Radiofrequency Ablation: This minimally invasive procedure uses radiofrequency energy to reduce the size of the tonsils or adenoids.
For patients with obstructive sleep apnea due to enlarged tonsils and adenoids, treatment may also include:
Continuous Positive Airway Pressure (CPAP): A CPAP machine delivers a steady stream of air to keep the airway open during sleep.
Oral Appliances: Dental devices can help reposition the jaw and tongue to improve airflow.
It's important to note that the cost of enlarged tonsils and adenoid treatment can vary significantly based on the specific procedures and interventions required. Surgical options tend to incur higher costs due to the need for anesthesia, hospital stays, and follow-up care. Always consult with a healthcare provider for a detailed estimate based on individual circumstances and treatment plans.
If left untreated, enlarged tonsils and adenoids can lead to various complications, including:
Obstructive Sleep Apnea: This serious condition can result in cardiovascular issues, daytime fatigue, and cognitive impairments.
Chronic Respiratory Issues: Mouth breathing can lead to respiratory problems and increase susceptibility to infections.
Recurrent Ear Infections: Blocked Eustachian tubes can result in fluid buildup in the ears, leading to recurrent infections and hearing loss.
Difficulty in Daily Activities: Pain and discomfort from enlarged tonsils and adenoids can affect quality of life, impacting work and social interactions.
While it may not be possible to prevent enlarged tonsils and adenoids entirely, several measures can help reduce the risk of developing complications:
Practice Good Hygiene: Regular handwashing and avoiding close contact with sick individuals can help reduce the risk of infections.
Manage Allergies: Identifying and managing allergens can prevent chronic inflammation of the tonsils and adenoids.
Avoid Smoking and Pollutants: Reducing exposure to smoke and environmental irritants can help protect respiratory health.
Regular Check-ups: Routine visits to healthcare providers can help monitor symptoms and catch any potential issues early on.
At Felix Hospital, we specialize in advanced treatments for Enlarged Tonsils and Adenoids in Adults. Our expert ENT surgeons in Noida, Dr. Arvinder Pal Singh, and Dr. Kunwar Parvez are renowned for their expertise in minimally invasive procedures. They utilize state-of-the-art laser technology to provide effective solutions for adult patients suffering from enlarged tonsils and adenoids. With years of experience and a commitment to patient-centered care, our specialists ensure optimal outcomes and faster recovery times.
Are you experiencing symptoms related to enlarged tonsils or adenoids? Click Here for more.
Enlarged tonsils and adenoids in adults can significantly impact quality of life and lead to various health complications. Understanding the causes, symptoms, and treatment options is essential for effective management. While conservative approaches may suffice in mild cases, surgical interventions may be necessary for more severe symptoms.
If you suspect you have enlarged tonsils or adenoids, consult a healthcare professional for a thorough evaluation and appropriate treatment options. Early intervention can help alleviate symptoms and improve overall well-being.
1. Can enlarged tonsils and adenoids affect adults?
ANS: Yes, enlarged tonsils and adenoids can occur in adults and lead to various health issues such as sleep apnea and difficulty swallowing.
2. What are the symptoms of enlarged tonsils and adenoids in adults?
ANS: Common symptoms include difficulty swallowing, persistent sore throat, snoring, sleep disturbances, and recurrent ear infections.
3. How are enlarged tonsils and adenoids diagnosed?
ANS: Diagnosis typically involves a medical history review, physical examination, imaging tests, and sometimes a sleep study.
4. What are the treatment options for enlarged tonsils and adenoids in adults?
ANS: Treatment options include conservative management, medications, and surgical options like tonsillectomy and adenoidectomy.
5. Can lifestyle changes help prevent enlarged tonsils and adenoids?
ANS: Yes, practicing good hygiene, managing allergies, avoiding smoking, and having regular check-ups can help reduce the risk of complications.

Obstructive Sleep Apnea (OSA) is a common but serious sleep disorder that affects millions of people worldwide. Characterized by repeated interruptions in breathing during sleep, OSA can lead to a variety of health complications if left untreated. Understanding the condition, its causes, symptoms, and treatment options is crucial for effective management and maintaining overall well-being. Diagnosis and treatment at the best ENT hospital in Noida can ensure the best care for OSA patients, addressing the root causes and offering advanced therapies to improve sleep quality and overall health. Let’s dive into everything you need to know about Obstructive Sleep Apnea, including its diagnosis, risk factors, and available therapies.
Schedule a consultation with our experienced sleep specialists today. Call now at +91 9667064100.
Obstructive Sleep Apnea occurs when the muscles in the throat relax excessively during sleep, causing the airway to become partially or fully blocked. This leads to repeated pauses in breathing (called apneas), often followed by a choking or gasping sound as the body tries to restart normal breathing. Each pause can last from a few seconds to more than a minute, significantly disrupting sleep and reducing oxygen levels in the blood.
Unlike Central Sleep Apnea (CSA), which involves a failure of the brain to signal muscles to breathe, OSA is primarily a mechanical issue involving the airway.
Several factors contribute to the development of OSA. Some of the most common causes include:
1. Excess Weight: Being overweight or obese is one of the most significant risk factors for OSA. Extra fat tissue around the neck can press on the airway and cause obstructions.
2. Anatomical Factors: The shape and size of a person's airway can predispose them to OSA. Individuals with a narrow throat, enlarged tonsils, or a large tongue may be more likely to develop the condition.
3. Age: OSA tends to be more common in older adults. As people age, muscle tone in the throat decreases, making it more likely for the airway to collapse during sleep.
4. Gender: Men are more likely to develop OSA than women. However, the risk for women increases after menopause.
5. Family History: Genetics can play a role in OSA. People with a family history of sleep apnea are more likely to develop the condition themselves.
6. Alcohol and Sedatives: These substances relax the muscles in the throat, increasing the likelihood of airway collapse during sleep.
7. Smoking: Smokers are more likely to develop OSA due to the inflammation and fluid retention in the upper airway caused by smoking.
8. Nasal Congestion: Chronic nasal congestion, whether from allergies or other causes, can make it harder to breathe through the nose, contributing to OSA.
OSA can manifest in a variety of ways, some of which may be easily noticeable, while others may go unnoticed without a proper diagnosis. Common symptoms of OSA include:
1. Loud Snoring: This is often one of the most recognizable symptoms of OSA. Snoring results from the vibration of tissues as air struggles to pass through a partially blocked airway.
2. Pauses in Breathing: Bed partners may notice that the individual stops breathing for short periods during sleep, often followed by a choking or gasping sound.
3. Excessive Daytime Sleepiness: Because OSA disrupts normal sleep cycles, individuals often feel fatigued during the day, despite spending a full night in bed.
4. Morning Headaches: OSA can lead to lower oxygen levels during the night, which may result in headaches upon waking.
5. Dry Mouth or Sore Throat: Breathing through the mouth due to a blocked airway can lead to dryness and discomfort.
6. Difficulty Concentrating: Lack of restful sleep can affect cognitive functions like concentration, memory, and decision-making.
7. Mood Changes: Individuals with OSA may experience irritability, depression, or anxiety due to chronic fatigue.
8. Restless Sleep: People with OSA often experience frequent awakenings during the night, although they may not remember them.
If left untreated, OSA can lead to a range of serious health problems. These include:
1. Cardiovascular Problems: OSA is closely linked to an increased risk of high blood pressure, heart attacks, strokes, and arrhythmias. Repeated drops in oxygen levels can put a strain on the cardiovascular system.
2. Diabetes: Sleep apnea has been associated with insulin resistance, which increases the risk of developing type 2 diabetes.
3. Daytime Fatigue: Chronic daytime sleepiness can impair concentration, reaction times, and overall performance, increasing the risk of accidents, especially while driving.
4. Metabolic Syndrome: OSA is associated with a cluster of conditions, including high blood pressure, abnormal cholesterol levels, and high blood sugar, all of which increase the risk of heart disease.
5. Liver Problems: People with OSA are more likely to have abnormal results on liver function tests, and their livers may show signs of scarring.
6. Impaired Immune Function: Poor sleep quality can weaken the immune system, making it harder for the body to fend off infections.
7. Mental Health Issues: The lack of quality sleep and chronic fatigue caused by OSA can contribute to the development or worsening of mental health conditions such as depression and anxiety.
Diagnosing OSA involves a thorough evaluation by a healthcare provider, often including a sleep specialist. Key diagnostic steps include:
1. Medical History: The doctor will ask about symptoms, medical history, and family history of sleep disorders.
2. Physical Examination: A physical exam may focus on the airway, looking for anatomical abnormalities like enlarged tonsils, a large tongue, or nasal obstructions.
3. Sleep Study (Polysomnography): The gold standard for diagnosing OSA is an overnight sleep study. This test monitors various physiological parameters during sleep, including brain activity, eye movements, heart rate, breathing patterns, oxygen levels, and limb movements. The results can help determine the severity of OSA and guide treatment decisions.
4. Home Sleep Apnea Testing: In some cases, a simpler version of a sleep study can be done at home using portable equipment to monitor breathing, oxygen levels, and heart rate.
The treatment of OSA depends on the severity of the condition and the underlying causes. Common treatment options include:
1. Continuous Positive Airway Pressure (CPAP)
CPAP therapy is the most common and effective treatment for moderate to severe OSA. It involves wearing a mask that delivers a constant stream of air pressure, keeping the airway open during sleep. Although it can take some time to get used to, CPAP is highly effective in reducing symptoms and improving quality of life.
2. Oral Appliances
For individuals with mild to moderate OSA, oral appliances may be recommended. These devices, worn in the mouth during sleep, help reposition the jaw and tongue to keep the airway open. They are often used when CPAP is not tolerated or preferred.
3. Lifestyle Changes
Certain lifestyle modifications can significantly reduce the severity of OSA:
Weight Loss: Losing excess weight can reduce fat deposits around the neck and improve airway function.
Exercise: Regular physical activity can help improve muscle tone and respiratory health.
Positional Therapy: Sleeping on your back can worsen OSA. Special devices or pillows can help keep individuals sleeping on their side, reducing airway blockages.
Avoiding Alcohol and Sedatives: Limiting the use of these substances can prevent excessive relaxation of the throat muscles.
4. Surgery
In some cases, surgery may be necessary to correct structural problems that contribute to OSA. Common surgical options include:
Uvulopalatopharyngoplasty (UPPP): This surgery involves removing excess tissue from the throat to widen the airway.
Genioglossus Advancement (GA): This procedure repositions the tongue muscle attachment to prevent airway obstruction.
Maxillomandibular Advancement (MMA): This involves moving the upper and lower jaw forward to enlarge the airway.
Tracheostomy: In severe cases, a tracheostomy may be performed to create an alternate airway through the neck.
5. Inspire Therapy (Upper Airway Stimulation)
Inspire therapy is a relatively new, FDA-approved treatment for moderate to severe OSA. It involves a surgically implanted device that stimulates the muscles of the airway to stay open during sleep. This option is typically recommended for patients who cannot tolerate CPAP.
While OSA may not always be preventable, certain measures can reduce the risk of developing the condition:
1. Maintain a Healthy Weight: Keeping a healthy weight through diet and exercise can reduce the risk of airway obstruction.
2. Sleep on Your Side: Sleeping on your back can exacerbate OSA, so side-sleeping is often recommended.
3. Avoid Alcohol and Sedatives: These substances relax throat muscles and can increase the risk of airway collapse.
4. Treat Allergies and Congestion: Managing chronic nasal congestion or allergies can help maintain a clear airway during sleep.
Dr. Arvinder Pal Singh (MBBS, MS) With extensive experience in ENT care, Dr. Arvinder Pal Singh specializes in the diagnosis and treatment of Obstructive Sleep Apnea (OSA).
Dr. Kunwar Parvez (MBBS, MS) Dr. Kunwar Parvez is the best ENT surgeon in Noida his dedication to patient well-being and advanced treatment techniques make him an excellent choice for those seeking effective OSA management and relief from related symptoms.
Obstructive Sleep Apnea is a serious condition that can have far-reaching consequences if left untreated. However, with proper diagnosis and a range of effective treatments, individuals with OSA can manage their symptoms, improve their sleep quality, and reduce the risk of complications. If you or someone you know is experiencing symptoms of OSA, such as loud snoring, frequent awakenings, or daytime fatigue, consult a healthcare provider for a proper evaluation and treatment plan. For those concerned about the ENT treatment cost in Noida, it’s important to seek consultation to understand the affordable and effective options available for managing OSA.
Take control of your health and prevent the long-term complications of untreated sleep apnea. Click Here to start your journey to better sleep and a healthier life!
1. What is Obstructive Sleep Apnea (OSA)?
ANS: OSA is a sleep disorder in which the airway becomes partially or completely blocked during sleep, causing breathing interruptions that can last from a few seconds to over a minute.
2. What are the common symptoms of Obstructive Sleep Apnea?
ANS: Common symptoms include loud snoring, pauses in breathing during sleep, gasping or choking, daytime sleepiness, morning headaches, dry mouth, and difficulty concentrating.
3. How is Obstructive Sleep Apnea diagnosed?
ANS: OSA is diagnosed through a sleep study (polysomnography), which monitors your breathing, oxygen levels, heart rate, and other vital signs while you sleep. A home sleep apnea test (HSAT) may also be recommended in some cases.
4. Can lifestyle changes help manage OSA?
ANS: Yes, lifestyle changes such as losing weight, avoiding alcohol and sedatives, sleeping on your side, and maintaining a healthy sleep routine can help manage OSA, especially in mild cases.
5. What is the most common treatment for Obstructive Sleep Apnea?
ANS: The most common treatment for OSA is Continuous Positive Airway Pressure (CPAP) therapy, which delivers a steady stream of air to keep the airway open during sleep.
6. Is surgery necessary to treat Obstructive Sleep Apnea?
ANS: Surgery may be necessary in severe cases of OSA where other treatments are ineffective. Surgical options include Uvulopalatopharyngoplasty (UPPP) and Inspire therapy, among others.
7. What are the risks of untreated Obstructive Sleep Apnea?
ANS: Untreated OSA can lead to serious complications such as high blood pressure, heart disease, stroke, diabetes, and reduced quality of life due to chronic fatigue.

In the realm of modern medical advancements, laser technology has revolutionized ENT (Ear, Nose, and Throat) surgeries, offering precision, faster recovery, and less invasive procedures. For those suffering from airway obstructions, finding the best hospital for airway obstruction treatment is critical. Laser technology provides a breakthrough in treating various ENT disorders with unparalleled accuracy, minimizing risks, and ensuring effective outcomes. At the Hospital, you need specialists to leverage cutting-edge laser techniques to offer patients enhanced care and swift recovery.
Get in touch with Felix Hospital today to consult with our Top ENT Specialists by calling +91 9667064100.
The laser revolution in ENT surgeries refers to the integration of laser technology in treating ENT conditions. Unlike traditional methods, laser surgeries use concentrated beams of light to cut, vaporize, or remove abnormal tissue with precision. These techniques are especially effective in treating airway obstructions, chronic sinusitis, tonsillectomies, ear disorders, and even certain throat cancers. Laser technology offers a minimally invasive alternative, reducing recovery time and enhancing precision.
Several conditions make laser-assisted ENT Surgery the preferred treatment choice:
1. Airway Obstructions: Conditions like sleep apnea, nasal polyps, or vocal cord lesions can block the airway, requiring precise intervention.
2. Chronic Sinusitis: Infections that don’t respond to medication can be treated with laser surgery.
3. Tonsillitis: Recurrent infections often call for tonsillectomy, where lasers are used for precision removal.
4. Ear Disorders: Problems such as otosclerosis (hardening of the ear bones) can be managed using laser techniques.
Laser technology allows for extremely precise incisions and removal of tissues, minimizing damage to surrounding healthy tissues. This precision is vital in areas such as the vocal cords, where traditional surgery can lead to voice complications. With lasers, surgeons can perform delicate operations with high control, resulting in quicker recovery, reduced bleeding, and less postoperative pain.
1. Minimally Invasive: Laser surgery requires smaller incisions, translating to less tissue trauma.
2. Reduced Bleeding: Lasers cauterize blood vessels as they cut, reducing the need for sutures and minimizing blood loss.
3. Faster Recovery: Patients experience shorter recovery times due to the procedure's precision and minimally invasive nature.
4. Decreased Risk of Infection: Smaller wounds and less tissue damage lower the risk of postoperative infections.
5. Shorter Hospital Stays: Patients can often return home the same day or after a short hospital stay.
Diagnosis for ENT disorders typically begins with a comprehensive clinical examination, followed by imaging tests such as CT scans, MRIs, or endoscopic evaluations. For conditions like airway obstructions or sinus issues, these diagnostic tools help ENT specialists evaluate the severity and determine whether laser surgery is appropriate.
Once diagnosed, treatment plans are developed based on the patient's condition. ENT surgeries utilizing laser technology are precise and cater to the patient's specific needs. For example, treating nasal polyps or enlarged tonsils with lasers leads to more effective results than traditional methods. When considering ENT surgery, ENT surgery cost for laser revolution is competitive, with Felix Hospital offering affordable packages without compromising quality care.
At Felix Hospital, we take pride in having some of the best doctors for laser revolution in ENT surgery. Dr. Arvinder Pal Singh and Dr. Kunwar Parvez are highly skilled ENT specialists, renowned for their expertise in laser-assisted surgeries. They bring years of experience and are committed to delivering the highest level of patient care using the latest in medical technology.
Book your consultation with the best doctors at Felix Hospital today and discover the benefits of laser revolution in ENT treatments by Clicking Here.
The laser revolution in ENT Surgeries has dramatically improved treatment outcomes, offering patients a minimally invasive, precise, and effective solution for various ENT disorders. Whether you are suffering from chronic sinusitis, airway obstructions, or ear disorders, laser-assisted surgery offers numerous benefits, including faster recovery, reduced bleeding, and decreased risk of complications. Felix Hospital, with its state-of-the-art facilities and expert ENT specialists, ensures that you receive top-quality care tailored to your needs.
1. What conditions can be treated with laser-assisted ENT surgery?
Laser-assisted ENT surgery can treat a wide range of conditions, including chronic sinusitis, tonsillitis, nasal polyps, airway obstructions, and vocal cord lesions.
2. Is laser ENT surgery painful?
Due to its minimally invasive nature, laser ENT surgery results in less postoperative pain compared to traditional surgery. Recovery is generally faster and more comfortable for patients.
3. How long does recovery take after laser ENT surgery?
Recovery times vary depending on the procedure, but most patients experience quicker recovery with laser surgery, often returning to normal activities within a week or two.
4. What is the cost of ENT surgery with laser technology?
The cost of laser-assisted ENT surgery can vary depending on the specific condition and procedure. At Felix Hospital, we offer competitive pricing and comprehensive care.
5. Are there any risks or side effects associated with laser ENT surgery?
While laser ENT surgery is generally safe, as with any surgical procedure, there are potential risks. These may include temporary swelling, minor bleeding, or infection. However, laser surgery significantly reduces the likelihood of complications compared to traditional methods.
6. How do I know if I’m a candidate for laser-assisted ENT surgery?
Your ENT specialist will evaluate your condition through a physical exam and necessary diagnostic tests. Conditions like airway obstructions, nasal polyps, and vocal cord issues may be suitable for laser surgery, but the final decision will depend on your specific diagnosis and overall health.
7. What should I expect during the recovery period after laser ENT surgery?
Post-surgery, most patients experience mild discomfort and swelling, which subsides in a few days. Your specialist will provide post-operative care instructions, and patients can usually return to daily activities much sooner than with traditional surgeries.

Have your tonsils removed through surgery. A procedure known as tonsillectomy, Is quite common. Is often done to address issues like chronic infections or obstructive sleep apnea related to the tonsils themselves. It's important to understand the ins and outs of Tonsil surgery. What the tonsils are all about and how to get ready, for the procedure includes knowing the risks involved and what costs you might expect. This blog post aims to walk you through the details of tonsil surgery so that you can feel prepared and informed about what lies ahead.
For those considering tonsil surgery, it's important to choose the right facility. Felix Hospital is recognized as the Best Hospital for Tonsil Surgery, offering state-of-the-art care, experienced surgeons, and personalized treatment plans tailored to each patient’s needs.
Feel free to reach out to our team, for guidance and assistance as you navigate through your treatment process! Contact us today at +91 9667064100.
The tonsils are a pair of oval-shaped tissues situated at the rear of the throat and play a role in the body's defense against infections. They can cause issues, like difficulty breathing or intense throat discomfort when they are frequently infected or swollen. Tonsillectomy is the surgery performed to eliminate the tonsils and is commonly advised for those experiencing repeated tonsil infections or obstructive sleep apnea.
Before moving with tonsil surgery it is crucial to conduct a thorough diagnosis first as part of the standard procedure:
Proper preparation is vital for a smooth tonsillectomy experience:
1. Pre-Surgical Consultation: Schedule a meeting, with your surgeon to go over the operation details and any potential risks involved well as what to expect during recovery.
2. Medical History: Inform the physician about your own or your child's medical background including health issues and allergies to medications or anesthesia used in previous procedures.
3. Avoid Certain Medications: Consider refraining from taking medications before the surgery, such, as blood thinners to reduce the risk of excessive bleeding during the procedure.
4. Pre-Operative Instructions: Follow guidelines on when to stop eating and drinking before surgery, typically 8-12 hours prior.
5. Arrange Post-Operative Care: Ensure that there is someone to help you or your child after the operation for proper care, during the healing phase because support will be necessary.
6. Prepare for Recovery: Make sure you have plenty of food and cold drinks ready for your recovery, after surgery, and set up a cozy resting area at home.
Recovering post a tonsil removal surgery is a stage in the medical procedure that demands careful consideration to promote ideal healing and ease of recovery process ahead. Here is an elaborate insight, into what one can anticipate during the recuperation timeframe:
Maintaining follow-up appointments with your healthcare provider is crucial, for monitoring the healing process after surgery. During these visits, your doctor will examine the site address any worries you may have, and make sure that your recovery is going well. If you experience any symptoms or complications your healthcare provider will offer advice on how to handle them effectively.
By adhering to these tips, for recovery post tonsil surgery, you can contribute to making the healing process more efficient and quicker.
While tonsil surgery is generally safe, it does carry some risks, including:
The Tonsil Surgery treatment cost may differ depending on factors such as the hospital chosen and the fees charged by the surgeon as well, as any extra procedures needed for the treatment. The typical cost usually falls within the range of ₹30k to ₹60k. It's advisable to reach out to the hospital or healthcare provider for a quote and to verify whether your insurance provides coverage for this surgery.
For more information about tonsil surgery or to schedule a consultation with one of our experienced ENT specialists, Contact Us Today at +91 9667064100.
Getting your tonsils removed can bring a lot of relief to people dealing with recurring tonsillitis or sleep apnea issues that block the airways during sleep periods. To be well prepared for the surgery and weigh the risks and expenses involved thoroughly is crucial before deciding to go through with it. It's important to seek advice, from a trusted healthcare to get personalized care that suits your specific circumstances best.
1. What are the common reasons for needing a tonsillectomy?
ANS: Common reasons include chronic tonsillitis, obstructive sleep apnea, and enlarged tonsils causing breathing or swallowing difficulties.
2. How long does a tonsillectomy procedure take?
ANS: The procedure typically takes about 30 to 60 minutes.
3. Is tonsillectomy performed under general anesthesia?
ANS: Yes, tonsillectomy is usually performed under general anesthesia, meaning the patient will be asleep during the surgery.
4. What is the typical recovery time after a tonsillectomy?
ANS: Most patients recover within 1 to 2 weeks, though full recovery may take up to 2 weeks.
5. Can tonsillectomy be performed on children?
ANS: Yes, tonsillectomy is commonly performed on children, especially if they have recurrent tonsillitis or obstructive sleep apnea.
6. Are there any long-term effects after having a tonsillectomy?
ANS: Generally, there are no long-term effects, but some patients may experience changes in their immune response.
7. What are the signs of complications after tonsil surgery?
ANS: Signs include severe pain, excessive bleeding, high fever, or difficulty breathing.
8. Will I need to follow a special diet after the surgery?
ANS: Yes, a diet of soft foods and plenty of fluids is recommended to help with recovery and reduce irritation.
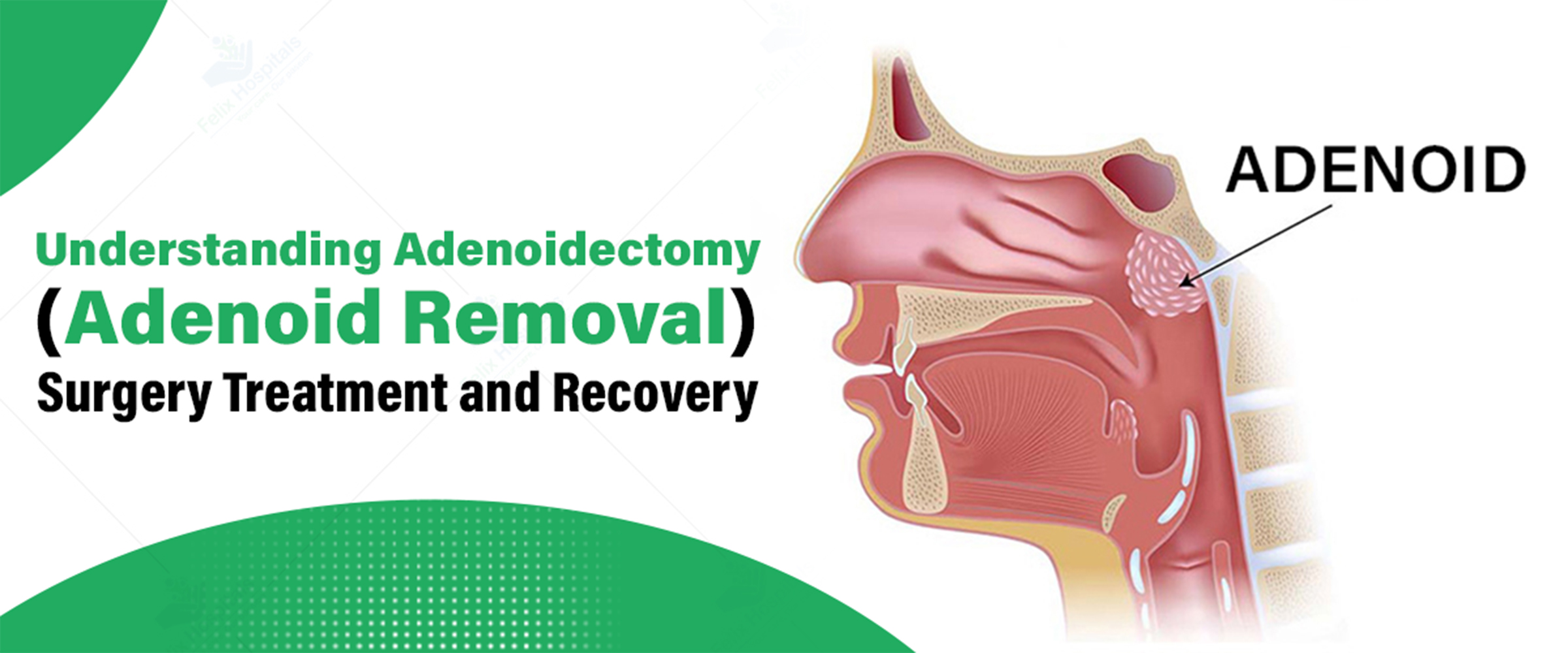
Adenoidectomy surgery is a well-established procedure designed to address issues related to enlarged adenoids, which are lymphatic tissues located at the back of the nasal cavity. When these adenoids become enlarged, they can lead to significant breathing difficulties and other health complications. This article provides a comprehensive overview of adenoidectomy, including its objectives, detection methods, treatment alternatives, and recovery process. It aims to give you a clear understanding of what to expect if this surgery is recommended. For those seeking the Best Hospital for adenoid removal surgery, this guide will help you make informed decisions about your care.
Contact us today at +91 9667064100 to schedule a consultation and learn more about your options.
Adrenalectomy is an operation designed to extract the adenoids situated at the rear of the throat above the palate ceiling level. This surgery is usually advised in cases where the adenoids are inflamed or infected causing problems such as sinus infections, obstructive sleep apnea, or challenges, in nasal breathing. While it is commonly carried out in children adults may also require this procedure at times.
Diagnosing adenoid problems usually requires an approach to ensure precise assessment and planning for treatment needs. Here's an in-depth exploration of how the diagnostic process unfolds:
Medical History: The doctor will start by going through the patient's medical background which involves talking about any signs like regular ear infections, persistent stuffy nose, or trouble breathing through the nose. Recognizing how often these signs occur and how severe they are aids, in evaluating if the adenoids might be part of the issue.
Physical Examination: During the check-up phase of the process comes a detailed examination of the body's condition by the doctor. The physician will inspect the throat and nasal passages using an endoscope—a slender tube equipped with a light and camera to provide a close look, at the adenoids for evaluation of their size and health status. This assessment aids in determining if the adenoids are enlarged and potentially blocking the airway or causing related symptoms.
Imaging Tests: To get a look at the adenoids and how they affect nearby structures in more detail imaging tests like X-rays or other diagnostic studies of imaging might be carried out. These examinations assist in seeing the level of enlargement and any related issues giving important details, for planning surgery.
Additional Tests: Additional Examinations Required; On occasions, additional examinations might be needed to assess the functionality of the adenoids or to pinpoint any underlying issues that could be impacting the patient well being. These tests may involve evaluating the adenoid's influence, on ear function or other connected aspects.
By utilizing a combination of these approaches in healthcare settings medical professionals can precisely assess the necessity, for adenoidectomy and create a customized treatment strategy that aligns with the patient's situation and requirements.
Adenosine is usually done as a day surgery while the patient is fully asleep, with anesthesia to keep them comfortable during the procedure which usually includes:
Removal of Adenoids: The Adenoid removal surgeon takes out the adenoids by going through the mouth of making cuts, outside the body to reduce scarring and target the troublesome tissue effectively.
Minimally Invasive Techniques: Modern approaches, to adenoid removal procedures frequently involve the use of tools that aim to minimize pain and speed up the recovery process effectively.
Post-Operative Care: After the surgery is done and dusted by the team is over with it they give you a bunch of instructions for post-operative care that you have to follow religiously if you want to get back on your feet quickly. This includes tips, on how to deal with pain eat the right foods, and not overdo physical activities to ensure a speedy recovery.
The time, after having adenoids removed usually includes the following elements:
Hospital Stay: After surgery, at the hospital, most patients can go home the same day; however in certain situations, they may need to stay overnight for observation to ensure their recovery is going well and to watch out for any possible issues that may arise.
Pain Management: Post-surgery pain can be alleviated through the use of prescribed medications and over-the-counter pain relievers, which play a role, in ensuring comfort and facilitating a faster healing process.
Diet: During the stages of recovery, it's best to opt for gentle foods and drink lots of liquids to avoid irritating the surgical area and promote healing.
Activity Restrictions: Following surgery guidelines is crucial for a recovery process and minimizing complications and ensuring proper healing at the surgical site includes refraining from intense activities as, per the surgeon's advice.
Follow-Up Appointments: Regular check-up visits with your healthcare provider are really important, for keeping track of how you're healing and dealing with any worries that come up along the way to make sure you're recovering as planned.
Schedule a Consultation today to discuss your concerns and explore treatment options. Click Here for more information.
Adenoidectomy is a crucial surgery that can provide significant relief for individuals dealing with issues related to enlarged adenoids. Understanding the diagnosis process, available treatment options, and what to expect during recovery can greatly assist in making informed decisions about your health or that of your child. For tailored guidance and professional medical attention, it is advisable to consult with a specialist who can determine the most appropriate treatment plan. Additionally, considering the adenoid removal surgery treatment cost is important for planning and managing expenses effectively.
1. What are the common symptoms that indicate a need for adenoidectomy?
Symptoms can include chronic nasal congestion, frequent sinus infections, difficulty breathing through the nose, snoring, and sleep apnea.
2. Is adenoidectomy a painful procedure?
While some discomfort is expected, pain can be managed with medications. Most patients experience minimal pain and recover quickly.
3. How long does it take to recover from adenoidectomy?
Recovery time can vary, but most patients feel better within one to two weeks. Following the surgeon’s post-operative care instructions can aid in a faster recovery.
4. Are there any risks associated with adenoidectomy?
As with any surgery, there are risks, including infection, bleeding, and reactions to anesthesia. However, complications are rare and the procedure is generally safe.
5. Can adenoidectomy be performed on adults?
Yes, while it is more common in children, adults may also undergo adenoidectomy if they experience significant symptoms or complications.
6. What should I do if I experience complications after the surgery?
Contact your healthcare provider immediately if you experience severe pain, excessive bleeding, high fever, or difficulty breathing.
7. Will adenoidectomy affect my child’s speech or swallowing?
Most children do not experience significant changes in speech or swallowing after the procedure. If concerns arise, consult with your healthcare provider for guidance.
8. How can I prepare my child for adenoidectomy?
Explain the procedure in simple terms, reassure them, and follow the pre-operative instructions provided by the healthcare team. It can also help to prepare a comfortable recovery area at home.

Tonsils are small, oval-shaped glands located at the back of the throat that help to fight infections by filtering out bacteria and viruses that enter through the mouth and nose. However, when tonsils become frequently infected or enlarged, they can cause significant discomfort and complications.
In such cases, the coblation technique might offer a modern and minimally invasive solution. Many facilities in Noida, including the Best tonsillitis treatment hospital in Noida, offer the coblation technique at an affordable cost, making it an accessible option for all.
Tired of recurring tonsil stones? Call +91 9667064100 to explore tailored treatment options straight from our ENT experts.
The coblation technique is a modern tonsil stones removal surgery procedure used for removing or shrinking tonsil tissue with precision and minimal discomfort. It uses radiofrequency energy to create a low-temperature plasma field that gently dissolves the tissue, rather than burning it. This approach reduces pain, minimizes bleeding, and speeds up recovery compared to traditional methods, making it a more comfortable and efficient option for those needing tonsil surgery.
The coblation technique uses radiofrequency energy to gently dissolve the tonsils instead of using heat to cut through tissue. Here’s a step-by-step overview of the coblation procedure, giving you a clear understanding of how it works;
1- Administering Anesthesia
First, your doctor will administer general anesthesia to ensure you are completely asleep and comfortable during the procedure.
2- Setting up device
Then the surgeon sets up a coblation device, which contains an electrode that will deliver radiofrequency energy to the tonsils.
3- Creating the Plasma Field
The radiofrequency energy then forms a plasma field around the tonsil tissue. This plasma field operates at a low temperature, making it gentle on the tissues.
4- Removing the Tissue
Using the coblation device, the surgeon carefully removes or reduces the tonsil tissue through the mouth. The device's precision ensures only the targeted tissue is affected.
5- Controlling Bleeding
The low temperature set up through coblation device helps control bleeding by sealing off blood vessels as the tissue is removed.
The procedure for coblation is speedy and effective, making it an excellent choice for addressing tonsil stones. Performed by a skilled Tonsil stones removal doctor, the technique can offer precise results and typically involves minimal recovery time.
Coblation is an effective technique used to treat various conditions related to the tonsils and throat. Here are some common conditions that can be treated using coblation technique:
Chronic Tonsillitis: This is when the tonsils, which are located at the back of your throat, stay swollen and inflamed for a long period of time which often causes a sore throat, bad breath, and trouble swallowing anything.
Enlarged Tonsils: This happens when the tonsils become larger than its normal size. This makes it hard to breathe or swallow, and might lead to frequent infections or snoring as well.
Recurrent Tonsil Stones: These are small, hard deposits of bacteria, dead cells, and other debris that form in the tonsils and keep coming back. They can cause bad breath and discomfort in the throat.
Tonsillar Hypertrophy: This is a condition where the tonsils are unusually large. It can cause breathing problems, difficulty swallowing, or frequent infections.
If you experience any of these conditions, it is advisable to seek medical treatment preferably from the best tonsil stones removal hospital as the experts there can assist you seeking the most appropriate treatment as per your condition.
The coblation technique has emerged as a highly effective method offering several notable benefits over traditional approaches. Here are some key advantages of the coblation technique:
Less Pain: Coblation often causes less post-operative pain compared to traditional methods because it is less invasive and causes less damage to surrounding tissues.
Quicker Recovery: Patients typically experience a faster recovery time since the procedure is less traumatic to the tissues.
Reduced Bleeding: This technique works at a lower temperature that seals blood vessels which further reduces bleeding and lowers the risk of complications.
Precision: Coblation allows for precise removal of tissue with minimal impact on adjacent areas, which helps in achieving better outcomes and reducing the risk of damage to nearby structures.
Dr. Arvinder Pal Singh
Dr. Arvinder Pal Singh is a renowned ENT specialist with extensive experience in treating tonsil-related issues. Known for his advanced surgical techniques and patient-centered care, he provides effective solutions for both chronic tonsillitis and tonsil stones.
Dr. Kunwar Parvez
Dr. Kunwar Parvez is a leading ENT physician specializing in the management of tonsil conditions. With a focus on innovative treatments and compassionate care, Dr. Parvez offers personalized approaches to tackle tonsil problems.
Coblation is often considered the Best Choice for Tonsil Treatment due to its precision, minimal invasiveness, and effective results. By using a low-temperature plasma field, coblation removes tonsil tissue with minimal damage to surrounding structures, leading to reduced pain and a quicker recovery. The technique's ability to seal blood vessels during the procedure helps in minimizing bleeding and complications. Overall, coblation offers a balance of effectiveness and patient comfort, making it a preferred option for treating various tonsil conditions.
Looking for relief from tonsil pain? Reach out to us at +91 9667064100 for effective solutions and compassionate care!
What is the principle of coblation?
Coblation uses radiofrequency energy and saline solution to create a plasma field that gently removes or ablates tissue. This method is less invasive than traditional techniques, causing minimal heat damage to surrounding tissues.
What is the difference between diathermy and coblation?
Diathermy uses high-frequency electrical currents to generate heat for tissue removal, while coblation employs a plasma field created by radiofrequency energy and saline, reducing heat damage and offering more precise tissue removal.
Is the coblation procedure painful?
The procedure itself is typically performed under local anesthesia, so most patients experience minimal pain during the process. Some discomfort or soreness may occur afterward, but this is usually manageable with over-the-counter pain relief.
How much does a coblation treatment cost?
Tonsil stones removal surgery cost can vary widely based on the procedure, location, and healthcare provider. It’s best to consult with your provider for an accurate estimate and check if your insurance covers the treatment.
How long does the coblation procedure take?
Coblation procedures generally take between 30 minutes to an hour, depending on the specific condition being treated and the area being addressed. The duration can vary based on individual circumstances.
Are there any risks or side effects associated with coblation?
Risks are minimal but can include infection, bleeding, or temporary discomfort. Most side effects are mild and short-lived. Always discuss potential risks with your healthcare provider before undergoing the procedure.
What is the recovery time like after a coblation procedure?
Recovery time is usually quick, with many patients resuming normal activities within a few days. Some minor discomfort or swelling may occur, but these symptoms generally resolve within a week or so.

Adenoids, while often overlooked, play a crucial role in our body's immune system. These small patches of tissue, located at the back of the nasal cavity, are part of the body's first line of defense against inhaled pathogens. However, when adenoids become enlarged, they can cause a range of uncomfortable symptoms and health issues, particularly in children. This blog post will help you understand the intricacies of enlarged adenoids, exploring their symptoms, causes, treatment options, and associated costs.
Seeking Effective Treatment of Enlarged Adenoids? Call +91 9667064100 to schedule your consultation today!
Before we look into enlarged adenoids, it's important to first understand what adenoids are and what they do in the body. Knowing their role will help in better understanding of their treatment.
Adenoids are small, soft lumps of tissue located at the back of the nasal cavity, just above the roof of the mouth. They are part of the lymphatic system, which helps fight infections. Adenoids work alongside the tonsils to help protect the body from germs and bacteria.
The primary role of adenoids is to:
1. Trap bacteria and viruses entering through the nose
2. Produce antibodies to help fight infections
3. Aid in the development of the immune system, especially in young children
Adenoids are usually most prominent during childhood and start to shrink around ages 5 to 7. By the time a person reaches adulthood, the adenoids often become very small or disappear altogether. However, in some cases, adults may still have remnants of their adenoids.
Enlarged adenoids, or adenoid hypertrophy, happen when the adenoid tissue swells and grows larger than usual. This can occur due to infections, allergies, or other factors, causing the adenoids to become bigger than their normal size.
Enlarged adenoids are most commonly seen in children, especially between the ages of 3 and 7. However, they can also affect people of any age, including adults, although this is less common.
When adenoids become enlarged, they can block the nasal airways and the Eustachian tubes, which connect the middle ear to the throat. This blockage can cause breathing difficulties, nasal congestion, and ear infections or problems with hearing.
The symptoms of enlarged adenoids can vary in severity and may include:
Breathing Difficulties
Nasal Issues
Ear Problems
Sleep Disturbances
Other Symptoms
It's important to note that these symptoms can also be indicative of other conditions. Therefore, a proper medical evaluation is crucial for an accurate diagnosis.
Several factors can contribute to the enlargement of adenoids. Some of the common factors for enlargement of adenoids include:
Infections
Infections, whether viral or bacterial, can cause the adenoids to swell as they try to fight off germs. Common causes of these infections include cold viruses, Streptococcus bacteria, and the Epstein-Barr virus, which leads to mononucleosis.
Allergies
Allergic reactions can cause the adenoid tissue to become inflamed, which is especially common in children with hay fever, dust allergies, or pet allergies. This inflammation can lead to symptoms like nasal congestion and breathing difficulties.
Chronic Irritation
Exposure to irritants can lead to adenoid enlargement over time. These irritants include air pollution, secondhand smoke, and chemical fumes. Prolonged exposure to such environmental factors can cause the adenoids to swell, potentially leading to breathing issues and other related problems.
Genetic Factors
Some individuals may have a genetic predisposition to enlarged adenoids, meaning that their family history can influence the likelihood of experiencing this condition. If parents or siblings have had issues with enlarged adenoids, there may be an increased risk of similar problems occurring.
Hormonal Changes
Hormonal fluctuations can sometimes cause adenoid enlargement. As the body undergoes various changes during the developmental stage, hormonal shifts may affect the adenoids, leading to swelling or increased size.
Diagnosing enlarged adenoids generally involves several key steps:
1. Medical History
The doctor will ask about symptoms, their duration, and whether there is a family history of similar conditions to understand the background and possible causes.
2. Physical Examination
A thorough physical exam will include checking the throat and ears. Since adenoids are not directly visible through the mouth, this step helps assess any related issues.
3. Nasal Endoscopy
A nasal endoscopy may be used, where a thin, flexible tube with a camera is gently inserted through the nose to directly view the adenoids and assess their size and condition.
4. X-ray
A lateral neck X-ray may be ordered to visualize the size and shape of the adenoids, providing a clear picture of any enlargement.
5. Sleep Study
If sleep apnea is suspected due to adenoid enlargement, a sleep study, or polysomnography, may be recommended to evaluate breathing patterns and other sleep-related issues.
Enlarged adenoids treatment varies based on the severity of symptoms and the underlying cause. Options range from conservative management to surgical intervention.
1-Watchful Waiting
For mild cases, especially in younger children, doctors may advise monitoring the condition. Often, adenoids will shrink naturally as the child grows.
2-Medications
Several medications can help manage symptoms:
3-Nasal Irrigation
Saline nasal sprays or rinses can help clear nasal passages and provide symptomatic relief.
If conservative treatments are ineffective or if symptoms are severe, surgery might be required. There are two main types of surgical options available:
1-Adenoidectomy
This procedure involves the surgical removal of the adenoids and is usually performed on an outpatient basis under general anesthesia.
2-Adenotonsillectomy
In some cases, it may be necessary to remove both the adenoids and the tonsils during the same surgery.
Following surgery, patients typically need to:
There could be numerous factors that affect adenoidectomy surgery cost in Noida. These include:
Geographic Location: The Cost of Treating Enlarged Adenoids can vary significantly based on where you live. Urban areas typically have higher medical fees due to increased demand and living costs, while rural areas may offer lower rates. Regional differences can also impact overall expenses.
Healthcare Provider: Costs can differ depending on whether you see a general practitioner or a specialist, such as an ENT (ear, nose, and throat) doctor. Specialists generally charge more due to their expertise, and providers with extensive experience or high reputations may also have higher fees.
Type of Treatment: Treatment costs vary based on whether you opt for conservative management or surgical intervention. Non-surgical options, like medication, are generally less expensive but may involve ongoing costs. Surgical treatment, such as adenoidectomy, is more costly and includes fees for the procedure, anesthesia, and post-operative care.
Presence of Complications: If complications arise, such as infections or extended recovery times, the overall cost can increase. Additional procedures or extended medical care can lead to higher expenses beyond the initial treatment.
Insurance Coverage: Insurance coverage can greatly influence your out-of-pocket costs. It's important to check what your insurance plan covers, including any co-pays, deductibles, or co-insurance. Some treatments may require pre-authorization, which can affect the cost and availability of care.
By understanding these factors, you can better anticipate and manage the expenses associated with treating enlarged adenoids.
Dr. Arvinder Pal Singh
Dr. Arvinder Pal Singh, MBBS, MS, stands as one of the best adenoidectomy doctors in Noida. He is a seasoned ENT specialist with over 15 years of experience in the field of ENT and Head and Neck Surgery. His extensive expertise encompasses a range of procedures and treatments, including Nasal Endoscopy, Functional Endoscopic Sinus Surgery (FESS), headache management, eardrum repair, ear wax removal, ear microsurgery, hearing deficiency assessment, ear lobe correction, and electrophysiology hearing. For expert care in addressing enlarged adenoids and other ear, nose, and throat issues, Dr. Singh offers comprehensive and skilled consultations.
Dr. Kunwar Parvez
Dr. Kunwar Parvez, MBBS, MS, is a highly skilled ENT specialist with extensive experience in treating a wide range of ear, nose, and throat conditions. His expertise includes advanced procedures such as Nasal Endoscopy, Functional Endoscopic Sinus Surgery (FESS), management of chronic sinus issues, and hearing assessments. Dr. Parvez is also adept at treating ear infections, eardrum repairs, and complex cases involving the head and neck. For personalized and expert care in ENT concerns, Dr. Kunwar Parvez provides comprehensive evaluations and treatments.
Enlarged adenoids, while common, can significantly impact a person's quality of life, especially in children. Understanding the symptoms, causes, and treatment options is crucial for managing this condition effectively. If you suspect that you or your child may have enlarged adenoids, visiting a specialized facility like the Adenoid Swelling Hospital in Noida can provide the necessary diagnosis and treatment. While the associated costs can be a concern, many treatment options are available, and insurance often covers necessary procedures. With proper diagnosis and treatment, the symptoms of enlarged adenoids can be effectively managed, allowing for improved breathing, better sleep, and overall enhanced well-being.
Don’t let enlarged adenoids hold you back! Call +91 9667064100 or simply click here for start feeling better today!
How do I know if my child has adenoid problems?
Common signs include frequent nasal congestion, breathing through the mouth, snoring, sleep disturbances, and frequent ear infections. Consult a pediatrician for a proper diagnosis if you notice these symptoms.
How can I naturally reduce my adenoids?
Natural methods include maintaining good hydration, using a humidifier to keep the air moist, and practicing good nasal hygiene. However, consult a healthcare professional for appropriate treatments and advice tailored to your situation.
At what age can adenoids be removed?
Adenoid removal, or adenoidectomy, can be performed at any age, but it's most commonly done in children between 3 and 7 years old. The procedure may be recommended if adenoid issues cause significant health problems.
Can adenoids go without surgery?
Yes, adenoids can sometimes shrink and improve on their own, especially in children as they grow older. Non-surgical treatments, like medications and lifestyle changes, may help manage symptoms, but surgical intervention might be necessary in persistent cases.
What happens if adenoids are left untreated?
Untreated adenoid problems can lead to chronic infections, difficulty breathing, sleep apnea, and potential impact on hearing. In severe cases, it may affect overall growth and development. Regular check-ups with a healthcare provider are essential.
Can Ayurveda cure adenoids?
Ayurveda offers various remedies and treatments aimed at reducing inflammation and boosting overall health. However, scientific evidence supporting Ayurvedic treatments for adenoids is limited. It’s best to consult both an Ayurvedic practitioner and a conventional healthcare provider.
Can adenoids affect the brain?
Enlarged adenoids can impact breathing and sleep, potentially leading to issues like poor concentration and behavioral problems. In severe cases, these effects may indirectly influence cognitive function. Consulting a healthcare professional is important for managing these risks.
Nasal Airway Obstruction (NAO) is a common condition affecting millions globally, requiring a clear understanding of its symptoms and causes for effective treatment. There are numerous experienced nasal airway obstruction surgeons in Noida, providing advanced options customized to each patient. Whether managing allergies, structural issues such as a deviated septum, or chronic sinus problems, seeking specialized care ensures thorough assessment and personalized treatment plans at top-notch facilities in Noida.
Struggling with Nasal Airway Obstruction? Contact us now to book an appointment! Call Now - +91 9667064100.
Nasal Airway Obstruction (NAO) is a condition characterized by a blockage in the nasal passages, making it difficult for individuals to breathe through their noses. This obstruction can significantly impact daily activities, including speaking, eating, and sleeping. NAO can arise from various causes, including structural abnormalities, inflammation, and external factors, leading to a range of symptoms that can affect a person's quality of life.
The nasal passages play a crucial role in filtering, humidifying, and warming the air we breathe. When these passages are obstructed, it can lead to inadequate airflow, which may result in discomfort and other health issues.
The symptoms of NAO can differ from person to person and vary in severity. The most commonly seen symptoms of NAO include:
If you experience one or more of these symptoms, such as persistent nasal congestion, difficulty breathing through your nose, or frequent sinus infections, it is advisable to seek medical attention promptly. Untreated nasal airway obstruction (NAO) can potentially lead to more serious health issues over time, impacting your quality of life and overall well-being.
Several factors can contribute to the development of nasal airway obstruction, including:
Deviated Septum: The septum is the cartilage wall that separates the nostrils. A deviated septum occurs when this wall is displaced, leading to one nasal passage being narrower than the other.
Enlarged Turbinates: Turbinates are structures within the nose that help warm and humidify inhaled air. When they become swollen due to allergies or infections, they can obstruct airflow.
Nasal Polyps: These are non-cancerous growths that can develop in the nasal passages, contributing to obstruction.
Allergic Rhinitis: Allergies to pollen, dust, pet dander, and other environmental factors can cause inflammation in the nasal passages, leading to congestion and obstruction.
Sinusitis: Chronic sinus infections can result in swelling and blockage of the nasal passages.
Poor Air Quality: Exposure to pollutants, smoke, and irritants can lead to inflammation and swelling of the nasal tissues.
Hormonal Changes: Hormonal fluctuations, such as those experienced during pregnancy, can also contribute to nasal congestion.
Understanding the underlying causes of NAO is crucial for determining the most effective treatment options and achieving long-term relief. A comprehensive evaluation by a healthcare professional ensures tailored treatment strategies that can significantly improve nasal airflow and overall quality of life.
While nasal airway obstruction itself is not typically life-threatening, it can lead to several complications if left untreated. Chronic nasal obstruction can result in:
Obstructive Sleep Apnea: A serious condition where breathing repeatedly stops and starts during sleep, leading to poor sleep quality and increased risk of cardiovascular issues.
Sinus Infections: Prolonged obstruction can hinder sinus drainage, resulting in recurrent sinus infections and associated symptoms.
Reduced Quality of Life: Difficulty breathing can affect daily activities, leading to fatigue, irritability, and decreased productivity.
Increased Risk of Respiratory Issues: Chronic nasal obstruction may contribute to respiratory problems, including asthma exacerbations.
It is essential to address NAO to prevent these potential complications and improve overall health and well-being.
Treatment for nasal airway obstruction varies depending on the underlying cause and severity of the obstruction. Common treatment options include:
Nasal Corticosteroids: These anti-inflammatory medications can help reduce swelling in the nasal passages and improve airflow.
Antihistamines: Useful for treating allergic rhinitis, antihistamines can alleviate symptoms caused by allergies.
Decongestants: These medications can temporarily relieve nasal congestion but should be used with caution to avoid rebound congestion.
Septoplasty: A surgical procedure to correct a deviated septum, improving airflow through the nasal passages.
Turbinate Reduction: This procedure reduces the size of enlarged turbinates, allowing for better airflow.
Nasal Polypectomy: Removal of nasal polyps to alleviate obstruction.
VivAer Treatment: A non-invasive procedure that uses low-temperature radiofrequency energy to reshape the nasal passages, improving airflow without the need for incisions.
Avoiding Allergens: Identifying and minimizing exposure to allergens can help reduce symptoms.
Humidifiers: Using a humidifier can help keep nasal passages moist, reducing congestion.
Nasal Irrigation: Saline nasal sprays or irrigation can help clear mucus and allergens from the nasal passages.
Consulting with a healthcare professional is essential to determine the most appropriate treatment plan based on individual needs, ensuring comprehensive evaluation and personalized care. This approach not only addresses immediate symptoms but also aims to manage underlying causes effectively, promoting long-term nasal health and overall well-being.
Nasal airway obstruction treatment Cost in Noida can vary significantly, influenced by factors such as the specific treatment chosen, the reputation and facilities of the healthcare provider, and the expertise of medical professionals.
On average, costs may range from approximately 40,000 to 45,000 INR at the lower end, up to 80,000 to 90,000 INR at the higher end of the spectrum.
For an accurate estimate tailored to individual treatment requirements, it is recommended to consult with healthcare providers in Noida. This ensures a detailed assessment and transparent discussion about the costs involved, facilitating informed decision-making for patients seeking effective relief from nasal airway issues.
Several factors can influence the cost of NAO treatment in Noida, including:
Type of Treatment: Surgical procedures generally cost more than medication management or non-invasive treatments.
Healthcare Facility: The reputation and location of the hospital or clinic can significantly impact treatment costs.
Surgeon's Experience: Highly experienced surgeons may charge higher fees for their expertise.
Pre- and Post-Operative Care: Costs associated with consultations, follow-up visits, and any necessary diagnostic tests can add to the overall expense.
Insurance Coverage: Patients with health insurance may have different out-of-pocket expenses based on their plan's coverage for specific treatments.
Understanding these factors can help patients make informed decisions regarding their treatment options, empowering them to actively participate in their healthcare journey and achieve optimal nasal function and comfort.
Felix Hospital in Noida is a leading nasal airway obstruction surgery Hospital in Noida known for its comprehensive approach to treating nasal airway obstruction. Here are several reasons to consider Felix Hospital for NAO treatment:
Expert Medical Team: The hospital boasts a team of Experienced ENT Specialists and best nasal airway obstruction surgeon in Noida dedicated to providing personalized care.
Advanced Treatment Options: Felix Hospital offers a range of treatment options, including both surgical and non-surgical interventions, ensuring that patients receive the most suitable care for their condition.
Advanced Facilities: The hospital is equipped with modern technology and facilities, ensuring high standards of care and patient safety.
Patient-Centered Care: Felix Hospital prioritizes patient comfort and satisfaction, providing a supportive environment throughout the treatment process.
Comprehensive Follow-Up Care: The hospital emphasizes the importance of follow-up care to monitor recovery and address any ongoing concerns.
Choosing the right healthcare provider is crucial for effectively managing nasal airway obstruction, and Felix Hospital stands out as a reliable option in Noida, renowned for its specialized care and commitment to patient well-being.
Nasal airway obstruction is a common condition that can significantly impact an individual's quality of life. Understanding its symptoms, causes, and treatment options is essential for effective management. With various treatment modalities available, including medications, surgical interventions, and non-invasive procedures, individuals suffering from NAO can find relief and improve their overall well-being.
If you or someone you know is experiencing symptoms of nasal airway obstruction, it is crucial to seek medical advice. Early diagnosis and appropriate treatment can prevent complications and enhance the quality of life.
1: What is the main cause of nasal obstruction?
The main causes of nasal obstruction include allergies, sinus infections, nasal polyps, deviated septum, turbinate hypertrophy, and structural issues in the nose.
2: Can a nasal obstruction cause difficulty breathing?
Yes, nasal obstruction can lead to difficulty breathing through the nose, causing discomfort and sometimes forcing mouth breathing.
3: How do you treat a blocked nasal passage?
Treatment options for a blocked nasal passage include saline nasal sprays, decongestants, antihistamines for allergies, nasal corticosteroid sprays, and in some cases, surgery to correct structural issues.
4: Can nasal obstruction cause bad breath?
Yes, chronic nasal obstruction can contribute to bad breath (halitosis) due to stagnant mucus and bacteria buildup in the nose and throat.
5: How long does nasal obstruction last?
The duration of nasal obstruction depends on the underlying cause. It can last from a few days (such as with a common cold) to chronic conditions that may require ongoing management.
6: Can nasal obstruction be cured?
Nasal obstruction can often be managed effectively with appropriate treatment. In some cases, such as structural issues, surgery may be required for long-term relief.
7: How do you prevent nasal obstruction?
To prevent nasal obstruction, practice good hygiene, manage allergies effectively, avoid irritants like smoke and strong odors, use a humidifier in dry environments, and seek prompt treatment for sinus infections or nasal congestion.
Cochlear implant surgery is a transformative procedure designed to restore hearing in individuals with severe to profound hearing loss. In Noida, a city renowned for its advanced medical infrastructure, the cost of cochlear implant surgery can vary widely based on several factors. Understanding these costs is crucial for effective planning and budgeting for the procedure.
Our dedicated team is here to provide expert care and support for your hearing needs. Call now - +91 9667064100.
Here is the typical costs associated with cochlear implant surgery in Noida:
| Minimum Cost | 3,00,000 |
| Maximum Cost | 12,00,000 |
| Average Cost | 8,00,000 |
Pre-Surgical Evaluation:
Surgical Costs:
Post-Surgical Costs:
The cost of cochlear implant surgery in Noida can vary based on several factors:
When selecting a healthcare facility for cochlear implant surgery in Noida, consider these key factors:
1. Compare Healthcare Providers: Research and compare costs between different hospitals. Choose facilities that offer the best value for your needs.
2. Leverage Insurance Coverage: Review your insurance plan to understand coverage for the implant, surgery, and post-operative care. Maximize your benefits.
3. Seek Financial Assistance: Explore patient assistance programs or financial aid options provided by hospitals or implant manufacturers.
4. Opt for In-Hospital Programs: Some hospitals offer comprehensive packages that include surgery, device, and rehabilitation at a discounted rate.
5. Plan for Follow-Up Care: Regular follow-ups and adjustments can prevent complications and reduce long-term costs.
1. Expert Medical Team: Felix Hospital features a team of Highly Skilled ENT Specialists and audiologists with extensive experience in cochlear implant surgery in Noida.
2. Advanced Diagnostic Technology: We use the latest diagnostic tools and imaging technologies to ensure accurate evaluation and planning.
3. Comprehensive Treatment Options: Our facility provides a range of services, including the latest cochlear implants, surgical procedures, and post-surgical rehabilitation.
4. Personalized Care Plans: We develop tailored treatment plans to meet each patient’s unique needs and goals.
5. Cutting-Edge Facilities: Our modern and well-equipped facilities are designed to offer comfort and high-quality care.
6. Multidisciplinary Approach: We employ a multidisciplinary approach, involving specialists from various fields to address all aspects of hearing restoration.
For more information about cochlear implant surgery and associated costs, or to Schedule a Consultation, call us at +91 9667064100.
The cost of cochlear implant surgery in Noida can fluctuate significantly depending on several key factors, including the type of implant used, the complexity of the surgical procedure, the choice of healthcare facility, and the extent of insurance coverage. Cochlear implants are a transformative solution for individuals with severe to profound hearing loss, and understanding the financial implications is essential for effective planning and budgeting.
1. What is the total cost of a cochlear implant?
The total cost of a cochlear implant can range between ₹3,00,000 to ₹12,00,000 in Noida. This includes the price of the implant itself, surgical costs, hospital stay, and post-operative care.
2. How serious is cochlear implant surgery?
Cochlear implant surgery is generally considered safe but involves risks, such as infection or device malfunction. It requires careful evaluation and a skilled surgical team to minimize complications.
3. Can a deaf person hear after a cochlear implant?
Yes, many individuals with severe to profound hearing loss experience significant improvements in hearing after a cochlear implant, though the degree of benefit can vary.
4. What are the disadvantages of cochlear implants?
Disadvantages can include surgical risks, the need for ongoing auditory therapy, potential device malfunctions, and the possibility of limited hearing restoration compared to natural hearing.
5. Can a deaf person hear again?
Cochlear implants can enable individuals who are profoundly deaf or severely hard of hearing to perceive sounds and improve their ability to understand speech, though the outcome can differ based on individual factors.
6. Is cochlear surgery painful?
The procedure is typically performed under general anesthesia, so patients do not experience pain during surgery. Post-operative discomfort is usually manageable with pain medication.
7. What is the best age for a cochlear implant?
Cochlear implants can be effective at various ages, but earlier implantation (often before 2 years of age) can enhance language development and auditory learning. Adults and older children can also benefit significantly from the implants.

Eardrum perforation, also known as tympanic membrane perforation, is a condition where there is a hole or tear in the eardrum. This can result from various causes, leading to symptoms that can significantly impact a person's hearing and quality of life. Timely and effective treatment is crucial to prevent complications. Felix Hospital in Noida offers comprehensive treatment options for eardrum perforation, including advanced surgical interventions.
Schedule your Consultation today by simply Clicking Here or calling us at +91 9667064100.
Table of Contents |
Several factors can causes of ear drum perforation, including:
1. Infections: Chronic ear infections can lead to a build-up of fluid in the middle ear, causing pressure that may perforate the eardrum.
2. Trauma: Direct injury to the ear, such as from a blow to the head, insertion of foreign objects, or sudden loud noises (acoustic trauma), can cause a perforation.
3. Barotrauma: Changes in air pressure, such as during air travel or scuba diving, can cause stress on the eardrum, leading to perforation.
4. Medical Procedures: In some cases, improper use of ear cleaning tools or the use of certain medical instruments during ear examinations can damage the eardrum.
Perforated eardrum symptoms can vary depending on the severity and cause of the perforation. Common symptoms include:
Hearing Loss: A noticeable reduction in hearing ability in the affected ear.
Ear Pain: Sudden, sharp pain that may subside quickly.
Drainage: Fluid or pus may drain from the ear, which can sometimes be bloody.
Tinnitus: Ringing or buzzing noise in the ear.
Vertigo: A spinning sensation that can lead to nausea and balance issues.
Treatment for a perforated eardrum depends on the size and location of the perforation, as well as the underlying cause. At Felix Hospital, we offer a range of treatment options tailored to each patient's needs:
1. Observation: Small perforations often heal on their own within a few weeks. During this period, keeping the ear dry and avoiding inserting objects into the ear is crucial.
2. Medications: Antibiotic ear drops may be prescribed to prevent or treat infection if the perforation resulted from an infection.
3. Eardrum Perforation Surgery: For larger or non-healing perforations, surgical intervention may be necessary. The most common procedure is tympanoplasty, which involves grafting a small patch of the patient's own tissue onto the eardrum to close the hole. Felix Hospital is a leading eardrum perforation surgery hospital in Noida, offering state-of-the-art surgical techniques and care.
Felix Hospital is renowned for its expertise in eardrum perforation surgery. Our team of experienced ENT specialists and surgeons are dedicated to providing the highest standard of care. We use advanced surgical techniques and equipment to ensure successful outcomes for our patients.
The Cost of eardrum perforation surgery in Noida can vary based on several factors, including the complexity of the procedure, the surgeon's experience, and the hospital's facilities. At Felix Hospital, we strive to provide high-quality care at competitive prices. The average cost of eardrum perforation surgery in Noida ranges from ₹30,000 to ₹70,000. For a detailed cost estimate tailored to your specific needs, we encourage you to consult with our specialists.
Felix Hospital stands out as one of the best hospitals for eardrum perforation treatment in Noida due to several key reasons:
1. Expert Team: Our team includes some of the best eardrum perforation treatment doctors in Noida, with extensive experience and Expertise in ENT care.
2. Advanced Facilities: We are equipped with state-of-the-art medical technology and surgical equipment to ensure the best possible outcomes.
3. Comprehensive Care: From diagnosis to post-operative care, we provide a holistic approach to ensure a smooth and successful recovery for our patients.
4. Patient-Centric Approach: We prioritize patient comfort and satisfaction, offering personalized care plans to meet individual needs.
At Felix Hospital, we're ready to assist you for Eardrum Perforation . Call now +91 9667064100.
1. Insurance Coverage: Ensure that your health insurance policy covers ENT procedures, including eardrum perforation surgery. This can significantly reduce out-of-pocket expenses.
2. Early Diagnosis: Early diagnosis and treatment can prevent complications that might require more extensive and costly interventions.
3. Preventive Care: Avoiding activities that risk ear trauma, such as inserting objects into the ear or exposing ears to sudden loud noises, can help prevent perforation.
Eardrum Perforation is a serious condition that requires timely and effective treatment to prevent complications such as hearing loss and chronic infections. At Felix Hospital, recognized as the best eardrum perforation treatment hospital in Noida, we offer comprehensive care, including advanced surgical options, to ensure the best outcomes for our patients. Our dedicated team of ENT Specialists and state-of-the-art facilities make us the top choice for eardrum perforation treatment in Noida. For more information or to schedule a consultation, please contact Felix Hospital today.
1. How do I know if my eardrum is perforated?
Answer: You might have a perforated eardrum if you experience symptoms like sudden sharp ear pain, hearing loss, ringing in the ear (tinnitus), drainage from the ear, or dizziness. If you suspect a perforated eardrum, see a doctor for a proper diagnosis.
2. Does a perforated eardrum heal itself?
Answer: Yes, in many cases, a perforated eardrum can heal on its own within a few weeks to a few months. However, larger perforations or those caused by infection might need medical treatment.
3. Is a perforated eardrum an emergency?
Answer: While a perforated eardrum is not usually a medical emergency, it is important to seek medical attention to prevent complications like infections or hearing loss. If you experience severe pain, discharge, or hearing loss, see a doctor promptly.
4. How long does it take for a hole in the eardrum to heal?
Answer: The healing time for a perforated eardrum can vary. Small holes often heal within a few weeks, while larger perforations might take a few months. Your doctor can give you a more specific timeline based on the size and cause of the perforation.
5. What is the best treatment for a perforated eardrum?
Answer: Treatment for a perforated eardrum may include keeping the ear dry, avoiding inserting anything into the ear, using prescribed ear drops to prevent infection, and sometimes taking pain relievers. In some cases, surgical repair, such as a patch or tympanoplasty, may be needed.
6. Can perforated eardrums heal on their own?
Answer: Yes, many perforated eardrums heal on their own without medical intervention. However, it is important to keep the ear dry and avoid inserting objects into the ear canal during the healing process.
7. Does a perforated eardrum need surgery?
Answer: Surgery is not always required for a perforated eardrum. Many perforations heal on their own. However, if the perforation does not heal or if it is causing significant hearing loss or recurrent infections, your doctor may recommend surgery.
8. How long does a perforated eardrum surgery take?
Answer: The surgery to repair a perforated eardrum, called a tympanoplasty, usually takes about one to two hours. The exact time can vary depending on the size and location of the perforation and the surgical technique used.
9. Is eardrum surgery a major surgery?
Answer: Eardrum surgery, or tympanoplasty, is considered a minor surgery. It is typically performed on an outpatient basis, meaning you can go home the same day. The procedure is usually safe and effective, with a relatively quick recovery time.
10. How much does it cost to fix a perforated eardrum?
Answer: The cost of eardrum surgery can vary widely depending on the country, the hospital, and whether or not you have insurance. In India, the cost of ear perforation surgery can range from INR 30,000 to INR 70,000. It is best to consult with a local hospital for a more accurate estimate based on your specific situation.