
Subscribe to our
Peptic ulcers are a common gastrointestinal condition that can cause significant discomfort and, if left untreated, lead to serious complications. These sores or open wounds develop in the lining of the stomach or the first part of the small intestine, known as the duodenum. Understanding the causes, symptoms, and effective treatment options for peptic ulcers is crucial for maintaining good digestive health. Don't delay - For the best peptic ulcer treatment in Noida, choose Felix Hospital, renowned as the best gastroenterology hospital in the region to receive effective care and prevent complications.
Call us now at +91 9667064100 to book your appointment and receive personalized care and effective treatment.
Peptic ulcers are a type of open sore that forms in the lining of the stomach or the duodenum, the first part of the small intestine. These ulcers are typically caused by a combination of factors, including the presence of the bacterium Helicobacter pylori (H. pylori) and the use of certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs).
The stomach and duodenum are normally protected by a thick, mucus-like layer that helps neutralize the acidic environment. However, when this protective barrier is compromised, the acidic stomach contents can damage the underlying tissue, leading to the formation of an ulcer.
There are two main types of peptic ulcers:
1. Gastric ulcers: These ulcers develop in the lining of the stomach.
2. Duodenal ulcers: These ulcers form in the first part of the small intestine, known as the duodenum.
The symptoms and treatment approaches for these two types of peptic ulcers may vary slightly, but the underlying causes and general management principles are similar.
The most common symptom of a peptic ulcer is a burning or gnawing pain in the upper abdomen, which may occur between meals or during the night. This pain is often described as a dull ache or a feeling of hunger, and it may be relieved temporarily by eating or taking antacid medications.
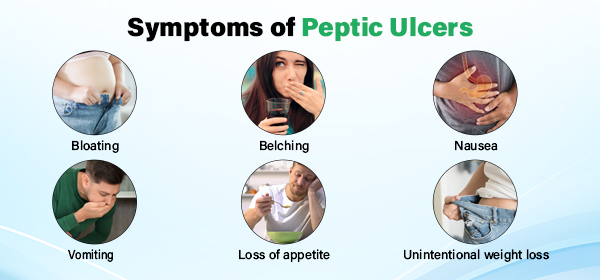
Other common symptoms of peptic ulcers include:
• Bloating
• Belching
• Nausea
• Vomiting
• Loss of appetite
• Unintentional weight loss
In some cases, peptic ulcers can cause bleeding, which may lead to the presence of dark or tarry stools (melena) or vomiting of blood (hematemesis).It's important to note that the severity and duration of symptoms can vary from person to person, and some individuals may even have asymptomatic ulcers that are only discovered during routine medical examinations.
The primary cause of peptic ulcers is the bacterium Helicobacter pylori (H. pylori), which can damage the protective lining of the stomach or duodenum. This bacterium is believed to be responsible for up to 60-80% of all peptic ulcers. H. pylori is a spiral-shaped bacterium that can burrow into the stomach lining, where it produces enzymes and toxins that can irritate and inflame the tissue. Over time, this can lead to the development of an ulcer.
In addition to H. pylori, certain medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), can also contribute to the development of peptic ulcers. NSAIDs, such as aspirin, ibuprofen, and naproxen, can irritate and damage the stomach lining, making it more susceptible to the formation of an ulcer.
Other factors that may increase the risk of developing peptic ulcers include:
• Excessive alcohol consumption
• Smoking
• Stress (although it is not a direct cause)
• Certain medical conditions, such as Zollinger-Ellison syndrome
It's important to note that the presence of H. pylori or the use of NSAIDs does not necessarily mean that an individual will develop a peptic ulcer. Other factors, such as the individual's immune response and the overall health of the digestive system, also play a role in the development of these ulcers.
In addition to the primary causes of peptic ulcers, such as Helicobacter pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs), there are several risk factors that can increase the likelihood of developing these sores or open wounds in the lining of the stomach or duodenum.
Excessive Alcohol Consumption: Excessive alcohol use can irritate and damage the protective lining of the stomach and duodenum, making them more susceptible to the development of peptic ulcers.
Smoking: Smoking has been shown to increase the risk of peptic ulcers. The chemicals in cigarette smoke can compromise the protective mechanisms of the stomach and duodenum, leading to the formation of ulcers.
Stress: While stress is not a direct cause of peptic ulcers, it can exacerbate the symptoms and contribute to the development of these ulcers. Chronic stress can weaken the body's defenses and make the digestive system more vulnerable to the damaging effects of stomach acid.
Certain Medical Conditions: Certain medical conditions, such as Zollinger-Ellison syndrome, can lead to an overproduction of stomach acid, increasing the risk of peptic ulcers.
Age: The risk of developing peptic ulcers increases with age, with the highest incidence occurring in older adults.
Family History: Individuals with a family history of peptic ulcers may have a higher genetic predisposition to developing these sores.
It's important to note that the presence of these risk factors does not necessarily mean that an individual will develop a peptic ulcer. Other factors, such as
Individual's overall health
Immune response
Lifestyle habits, also play a role in the development of these ulcers.
By being aware of these risk factors and taking proactive measures to maintain good digestive health, individuals can significantly reduce their risk of developing peptic ulcers.
To diagnose a peptic ulcer, your healthcare provider may perform various tests, including:
1.Upper endoscopy: This procedure involves inserting a thin, flexible tube with a camera (endoscope) down the throat and into the upper digestive tract to examine the stomach and duodenum for the presence of an ulcer.
2.Biopsy: During an endoscopy, a small sample of tissue may be taken from the ulcer site for further analysis to determine the underlying cause, such as the presence of H. pylori.
3.Blood, breath, or stool tests: These tests can detect the presence of H. pylori antibodies or the bacteria itself, which can help confirm the cause of the peptic ulcer.
4.Imaging tests: In some cases, your healthcare provider may order imaging tests, such as an upper gastrointestinal (GI) series or a CT scan, to get a better view of the digestive tract and identify any abnormalities.
Accurate diagnosis is crucial for determining the appropriate treatment plan, as the underlying cause of the peptic ulcer will dictate the most effective course of action.
The treatment for peptic ulcers depends on the underlying cause of the condition. If H. pylori is present, a combination of antibiotics and acid-reducing medications is typically prescribed to eradicate the bacteria and allow the ulcer to heal.
1. Antibiotics: If H. pylori is identified as the cause of the peptic ulcer, a combination of two or more antibiotics, such as amoxicillin, clarithromycin, or metronidazole, may be prescribed. The goal of antibiotic therapy is to eliminate the H. pylori infection and prevent the recurrence of the ulcer.
2. Acid-reducing medications: Proton pump inhibitors (PPIs), such as omeprazole, esomeprazole, or pantoprazole, are commonly used to reduce the production of stomach acid and promote the healing of the ulcer. These medications work by blocking the proton pumps responsible for acid secretion in the stomach.
3. H2 receptor antagonists: In some cases, H2 receptor antagonists, such as ranitidine or famotidine, may be prescribed to block the production of stomach acid and aid in ulcer healing.
If the peptic ulcer is caused by the use of NSAIDs, the treatment approach may involve discontinuing the offending medication or switching to a different type of pain reliever. In some cases, the addition of a PPI or H2 receptor antagonist may be necessary to help the ulcer heal.
In severe cases, or if the ulcer does not respond to medical treatment, surgical intervention may be required. Surgical options may include:
Ulcer removal (partial gastrectomy)
Procedures to reduce acid production (vagotomy)
Procedures to strengthen the lower esophageal sphincter (fundoplication)
It's important to follow the prescribed treatment plan and complete the full course of medication to ensure the effective eradication of H. pylori and the healing of the peptic ulcer. Failure to do so may result in the recurrence of the ulcer or the development of antibiotic-resistant strains of H. pylori.
Experience Special care at Felix Hospital. Contact us at +91 9667064100 to schedule an appointment.
To prevent the development of peptic ulcers, it is essential to adopt healthy lifestyle habits and take proactive measures to maintain good digestive health. Here are some key strategies for preventing peptic ulcers:
1. Maintain good hygiene: Practice proper handwashing, especially before handling food and after using the restroom, to reduce the risk of H. pylori transmission.
2. Avoid excessive use of NSAIDs: If you require pain relief, opt for alternative medications or use NSAIDs sparingly and under the guidance of your healthcare provider.
3. Quit smoking and limit alcohol consumption: Smoking and excessive alcohol use can increase the risk of developing peptic ulcers and delay the healing process.
4. Manage stress: While stress is not a direct cause of peptic ulcers, it can exacerbate symptoms and contribute to the development of ulcers. Engage in stress-reducing activities, such as exercise, meditation, or relaxation techniques.
5. Seek prompt treatment for H. pylori infection: If you are diagnosed with an H. pylori infection, follow the prescribed treatment plan to eradicate the bacteria and prevent the recurrence of peptic ulcers.
6. Maintain a healthy diet: Consume a balanced diet rich in fruits, vegetables, and whole grains, which can help support digestive health. Avoid spicy, acidic, or fried foods that may irritate the stomach lining.
7. Stay hydrated: Drink plenty of water to support the production of protective mucus in the stomach and duodenum.
By implementing these preventive measures, you can significantly reduce your risk of developing peptic ulcers and maintain a healthy digestive system.
Dr. Jagatjot Singh Gill is a proficient and committed gastroenterologist with over 11+ years of extensive experience. His expertise lies in diagnosing, treating, and managing a wide range of gastrology conditions and disorders. Committed to improving patient well-being, he endeavours to deliver exceptional care and customized treatment strategies designed to address the specific needs of every patient.
Peptic ulcers are common gastrointestinal issues that can cause discomfort and lead to serious complications if untreated. Understanding their causes, symptoms, and treatments is vital for digestive health. The primary cause is the bacterium Helicobacter pylori, which damages the stomach or duodenum lining. Certain medications, like NSAIDs, can also contribute to ulcers. Symptoms include upper abdominal pain, bloating, belching, nausea, vomiting, and sometimes bleeding. Diagnosis via endoscopy and biopsy is essential for proper treatment, which typically involves antibiotics and acid-reducing medications. Preventive measures include good hygiene, avoiding NSAIDs, quitting smoking, managing stress, and a healthy diet. If you suspect a peptic ulcer, seek medical attention promptly for diagnosis and treatment. With proper care, most peptic ulcers can be effectively treated and prevented from recurring.
1) Are peptic ulcers painful?
Ans. Yes, peptic ulcers are typically very painful, causing a burning or gnawing sensation in the stomach. This pain often worsens when the stomach is empty and can be temporarily relieved by eating certain foods or taking antacids.
2) How would I know if I have a peptic ulcer?
Ans. You might have a peptic ulcer if you experience symptoms like persistent stomach pain, bloating, heartburn, nausea, or vomiting. To confirm, a doctor may recommend an endoscopy, barium swallow, or testing for H. pylori infection.
3) What foods should I avoid eating if I have a peptic ulcer?
Ans. If you have a peptic ulcer, avoid spicy foods, alcohol, caffeine, acidic foods like citrus and tomatoes, and fatty or fried foods. These can irritate the stomach lining and exacerbate ulcer symptoms, delaying healing.
4) Do peptic ulcers go away on their own?
Ans. Peptic ulcers usually do not go away on their own and require medical treatment to heal properly. Without treatment, they can worsen, leading to complications such as bleeding, perforation, and stomach obstruction.
5) Which is the best peptic ulcer treatment hospital in Noida?
Ans. Felix Hospital in Noida is highly recommended for peptic ulcer treatment. It offers specialized gastroenterology services, experienced medical professionals, and advanced diagnostic facilities, ensuring comprehensive care for patients with peptic ulcers.